Spike Protein and Brain Injury
Those suffering from spike protein Post-Vaccine Syndrome and Long Haul Covid have found their brain to be profoundly impacted, and are seeking answers. Many patients talk of “brain fog”, which might include memory recall issues, word retrieval issues, unclear thinking, and difficulty focusing. However, the symptoms go well beyond brain fog.
In some corners of the internet, you may find discourse between patients dealing with anhedonia, depersonalization/derealization, depression, and anxiety. Additionally, you may even come across conversations about complete personality changes. You may be experiencing these things yourself. On the Side Effects with Dr. Josef podcast, Scott Marsland discusses why so many of the Post-Vaccine Syndrome injuries look like traumatic brain injuries.
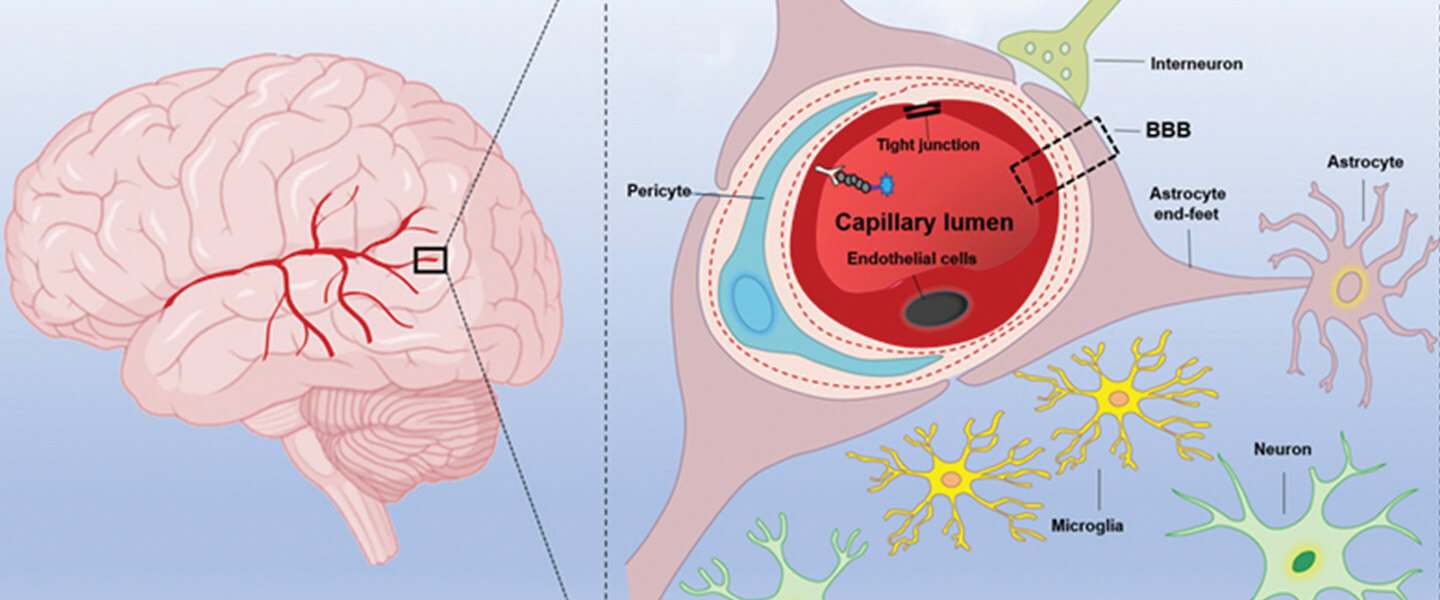
Even in the conventional medical system, there is now a significant body of research evidence demonstrating the various mechanisms by which the spike protein induces these brain-injury manifestations. If you peruse mainstream journals like Nature, you will find studies highlighting the ability of the spike protein’s S1 unit to cross the Blood Brain Barrier.
Here is a list of pathophysiological ways spike induces brain injury:
- Blood-Brain Barrier Disruption – binding to ACE2 receptors on endothelial cells, disrupting tight junctions and increases permeability; activating the RhoA signaling pathway, leading to the disassembly of the endothelial cell cytoskeleton and junction proteins; inducing the production of vascular endothelial growth factor (VEGF), a potent inducer of vascular permeability.
- Endothelial Damage – bind directly to fibrinogen, promoting the formation of proinflammatory blood clots (microthrombi) and contributing to systemic thromboinflammation, which can cause microvascular damage in the brain
- Neuroinflammation – directly activates glial cells (microglia and astrocytes), the brain’s resident immune cells, even without full viral replication in the brain parenchyma, which then release pro-inflammatory cytokines, especially interleukin-1β (IL-1β), which is neurotoxic and leads to bystander neuronal death
- Accumulation of Neurodegenerative Proteins – induce the aggregation and accumulation of proteins associated with neurodegenerative diseases, which are linked to synaptic dysfunction and neuronal loss
- Prion Formation – contains “prion-like” domains (PrDs) that can interact with amyloidogenic proteins in the brain, potentially accelerating their misfolding and contributing to neuroinflammation and neurodegenerative diseases
Foundations For Treating Spike Induced Injury
There is no shortage of avenues to attempt to treat the neurological symptoms of those suffering from Long Haul Covid and Post-Vaccine Syndrome. There are adaptogens, anti-inflammatory compounds, immunomodulatory compounds, and methods to support vascular health. A multi-pronged approach is key to addressing multiple pathophysiological mechanisms, as well as clearing the body and brain of spike protein.
When we look at therapeutic interventions, there are a couple things we consider:
- Efficacy
- Safety
- Degree of Impact
- Ability to address multiple issues at once.
One treatment checks all four boxes, and does so with gusto.
The History Of Low-Dose Ketamine
Ketamine was first synthesized in the 1960s as a general anesthetic and approved in 1970, by the FDA. In 2020, Brazilian researchers found a fungus called Pochonia chlamydosporia which produced ketamine naturally and found that it demonstrated potent anti-parasitic efficacy equivalent to Albendazole and Ivermectin.
In 2000 to present day, a number of studies have demonstrated the effect of Ketamine on psychiatric disorders:
- In 2000, psychiatrists at Yale figured out that sub-anesthetic doses of ketamine produced rapid anti-depressant effects. That discovery initiated the practice of using IV ketamine to treat depression
- In 2013, Brazilian researchers discovered that a low dose of sublingual ketamine (10 mg every 2- 7 days) led to full or clear responses in 77% of patients with treatment-resistant unipolar and bipolar depression.
- In this series of hundreds of patients, the patients received six treatments of 300mg rapidly dissolving tablets of ketamine. 48% of patients demonstrated a significant reduction in depression scores after three treatments and after 6 treatments, 72.4% demonstrated improvements in anxiety and depression scores.
- In another case series, 17 patients received 0.5mg/kg or 1mg/kg SLK every 7 or 14 days with 76% (13) of the subjects classified as responders.
Our Introduction To Low Dose Ketamine

Our clinical team is fortunate to have become colleagues with (and students of) two of the most clinically experienced psychiatrists at the leading edge of using Ketamine in clinical practice – Dr. Rachel Wilkenson and Dr. Mitch Leister. They have now been using sublingual low-dose Ketamine in the treatment of numerous mental illness conditions for 5 and 3 years respectively.
In both published and unpublished case reports and series, the results they have achieved in their patients is nothing short of revolutionary. For the first time in their 20 and 40 year careers, they have seen dramatic recoveries in mood disorders, including:
- Major Depressive Disorder
- Treatment-resistant depression
- Bipolar disorder
- Anxiety disorders (GAD, PTSD, OCD, etc.)
- Borderline personality disorder, and many other psychiatric conditions.
Here are a few pieces of their clinical and research work:
- In an abstract they presented at the World Congress of Psychiatry in Vienna in 2023 they reported that an incredible 96% of patients’ depression scores improved (27% in full remission, 37% with an over 50% improvement, and 32% with improvements between 7-49%) over an average of just 3.4 months.
- Another trial gave 5 days of SL ketamine to 329 patients and found 168 had achieved a significant response by Day 8. These patients then received 12 weeks of treatment at various dose levels or placebo. At 13 weeks, the highest dose (180mg) met the primary outcome of a large reduction in score on a depression scale, while 70.6% of the placebo group relapsed compared to only 42.9% of ketamine patients during the trial.
Largely because of Dr. Wilkinson, Dr. Leister, and others’ research and clinical work, Ketamine is now on all updated protocols for depression and bipolar disorder as of Fall of 2023, according to continuing medical education articles (FOCUS journal sponsored by the American Psychiatric Association). There is no set limitation on the duration that patients are able to be treated with Ketamine, and recently there have been articles released that indicate long-term use results in cognitive improvement over at least the duration of two years – longer studies are ongoing.
Psychoplastogen... We Say Neuroplastogen
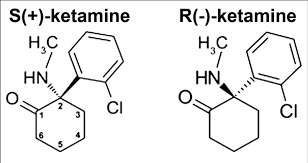
The importance of Ketamine is that it is a “paradigm shifter” given that it modulates a neurotransmitter called glutamate, rather than the neurotransmitters traditionally thought to be involved in and targeted by drugs for depression (i.e. deficiencies of serotonin, norepinephrine and/or dopamine).
Beyond its recognized glutamate modulating properties, Ketamine was found to be the prototype for a new class of medicines identified and named by a chemist in 2018 as “psychoplastogens” because of their ability to induce both structural and functional changes to the brain. However, for reasons you are about to see, we think Ketamine belongs under the name “neuroplastogen”.
At its simplest, ketamine can induce “brain growth” because at low doses (not at high doses):
- Stimulates the release of brain-derived neurotrophic factor (BDNF).
- Reduces excitotoxicity,
- Increases cerebral blood flow
- Up-regulates BDNF
- Increases nerve growth, dendritic spine density, and synapses
- Reduces neuroinflammation, apoptosis, cell death, and superoxide production.
As a result of up-regulated and stimulated release of BDNF, low-dose Ketamine also:
- Promotes the growth of new neurons (neurogenesis)
- Promotes the development of new synapses (synaptogenesis)
- As an antiparasitic, it even improves the composition of the gut microbiome
- Facilitates the re-myelination of neurons
- Reduces neuroinflammation
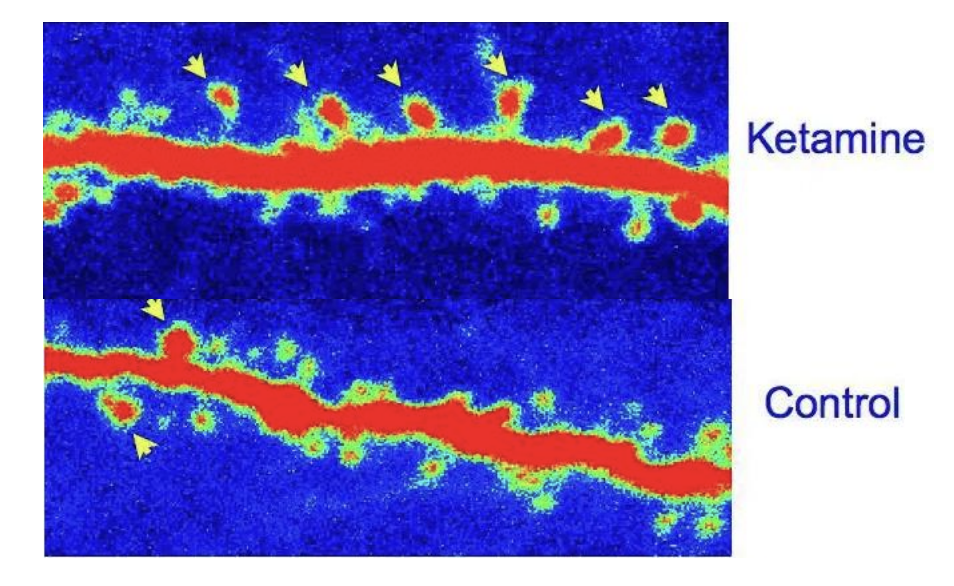
Here’s a picture taken with an electron microscope showing the effects of ketamine on a rat neuron. You can see all the extra bulbs or spikes that develop (yellow arrows) following treatment with ketamine. Each of these forms a new synapse.
Low-Dose Ketamine and Long Haul Covid, Post-Vaccine Syndrome, and ME/CFS
Under the tutelage of Dr. Wilkinson and Dr. Leister, we have confidently combined their findings on Low-Dose Ketamine, to our clinical findings with Long Haul Covid, Post-Vaccine Syndrome, and ME/CFS patients. In a year of implementing Low-Dose Ketamine treatments, we have seen promising results. Scott Marsland has written a few case studies on neurodegenerative disease, typical Long Haul ME/CFS related neurological presentation, and a variety of other patient cases.
If you recall, early in this piece, we highlighted a number of neurodegenerative pathways, neuronal destruction, and other neuroinflammatory pathways of spike protein. Then, we introduced the mechanisms of action of Low-Dose Ketamine. Mainly, these mechanisms of action reflected an uncanny ability to rebuild neuronal connections, reduce neuroinflammation, re-myelinate neurons, and develop new synapses.
So, how does this translate to our patients? We have seen any combination of the following:
- Improvement or cessation of dysautonomia
- Improvement or return to baseline energy levels and reduction or cessation of Post-Exertional Malaise (PEM)
- Improvement or return to executive functioning and cognition
- Improved GI symptoms, or return to normal GI function
- Improvement in mood, and/or reduction or cessation of depression, anxiety, and anhedonia
- Improvement or cessation of neuropathy
- Return of smell and/or taste
This is an incomplete list of clinical observations. But, it highlights some of the most significant types of improvements we see. We have witnessed patients go from disabled, to able-bodied. Furthermore, patients who are not quite disabled, report significant improvements allowing them to live more meaningful and full lives.
Conclusion
We have been extremely pleased with the results we have seen at Leading Edge Clinic. Of course, it is not as simple as just spoon-feeding Low-Dose Ketamine. Some patients with significant glutamate in the brain must first address these levels. While some patients see results immediately, others require time, patience, and careful titration.
Another significant factor that needs to be addressed is clearing the inflammatory, disruptive, and toxic spike protein. Low-Dose Ketamine does not do this. Of course, all of the information on the use of Low-Dose Ketamine in Long Haul Covid, Post-Vaccine Syndrome, ME/CFS, and neurodenerative diseases are purely clinical. Every case is different.
Nothing from this article should be construed as medical advice. Do not self treat. Find a capable and experienced clinician that can safely advise on the use of these therapies. Furthermore, ensure the clinician can deal with the full picture. Low-Dose Ketamine is a great therapy that helps on multiple layers of spike pathology. But, it is not a panacea. There is no panacea for multi-system complex illness.
Stay tuned as we expect more case studies from the front lines on patients treated with Low-Dose Ketamine.