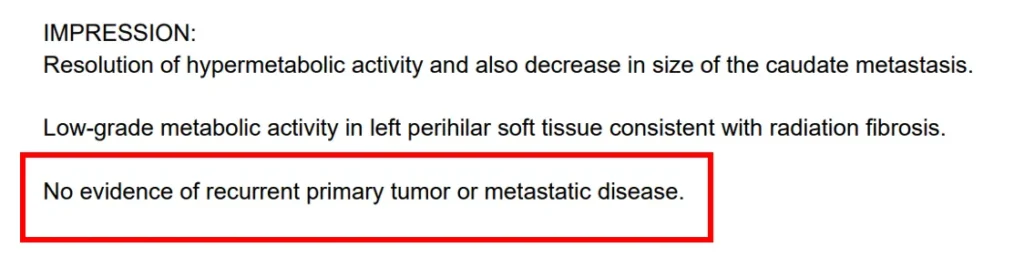
MCAS and Long Covid: The Connection & Treatment Options
Understanding Mast Cell Activation Syndrome in Post-Acute Sequelae of COVID-19 and Post-Vaccine Syndrome
_____
Table of Contents
- What is MCAS?
- The Link Between MCAS and Long Covid
- MCAS Symptoms in Long Covid Patients
- How MCAS is Diagnosed
- Why MCAS Treatment In Long Covid Requires Specialized Clinical Care
- When to Seek Specialized Care
- Patient Success Stories
- Frequently Asked Questions
____
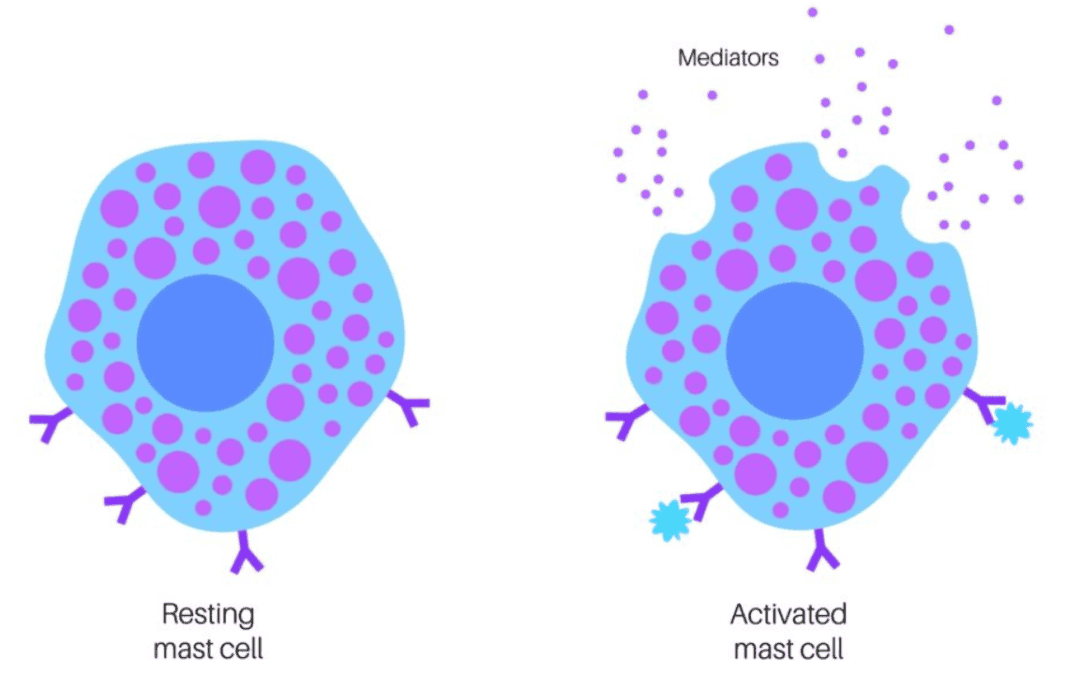
What is MCAS?
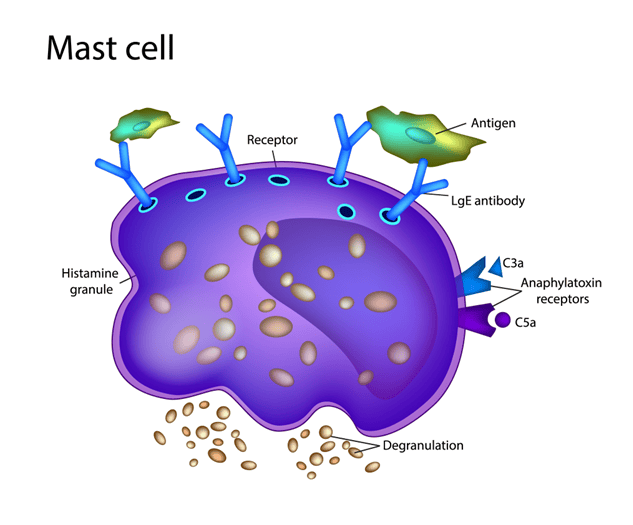
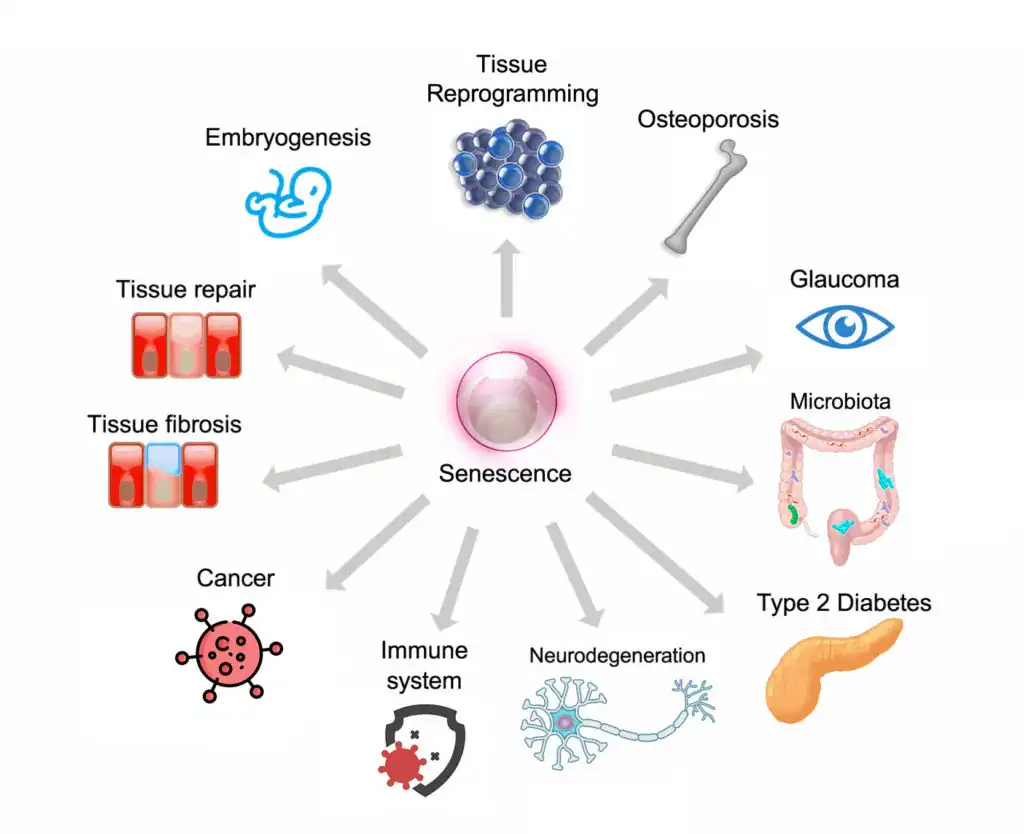
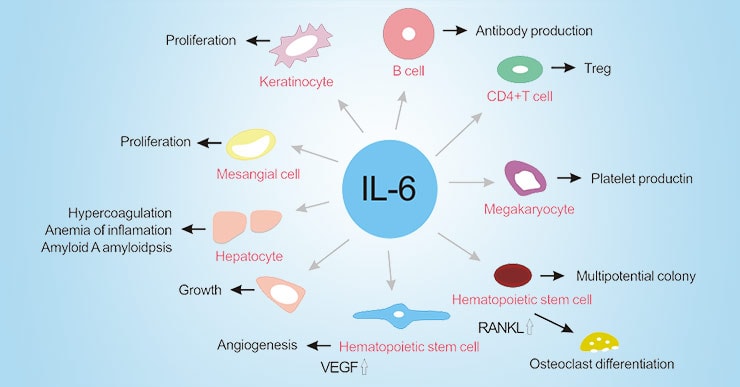
Mast Cell Activation Syndrome (MCAS) is a complex immune system disorder where mast cells—a type of white blood cell—release excessive amounts of chemical mediators like histamine, tryptase, and prostaglandins. These chemicals trigger widespread symptoms affecting multiple organ systems.
Unlike mastocytosis, where there’s an abnormal proliferation of mast cells, MCAS involves normal numbers of mast cells that behave abnormally, becoming hyperactive and releasing mediators inappropriately.
Key Characteristics of MCAS:
- Multi-system involvement: Symptoms affect skin, gastrointestinal, cardiovascular, respiratory, and neurological systems
- Episodic nature: Symptoms can come and go, often triggered by specific factors
- Variable presentation: No two MCAS patients present exactly the same way
- Response to treatment: Symptoms typically improve with mast cell stabilizers and antihistamines
____
The Link Between MCAS and Long Covid
The connection between MCAS and Long Covid (Post-Acute Sequelae of COVID-19 or PASC) and Post-Vaccine Syndrome has become increasingly recognized in the medical community. Research suggests that **30-50% of Long Covid patients** may have MCAS or MCAS-like symptoms.
Why Does COVID-19 Trigger MCAS?
Several mechanisms explain how SARS-CoV-2 infection can lead to mast cell activation:
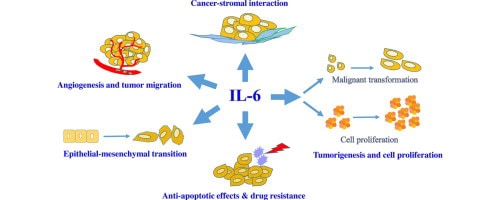
1. Direct Viral Activation
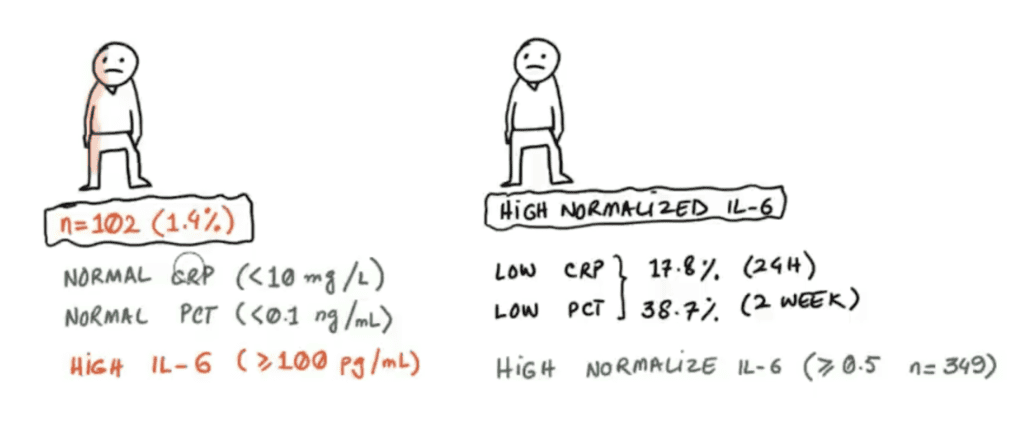
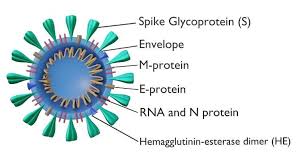
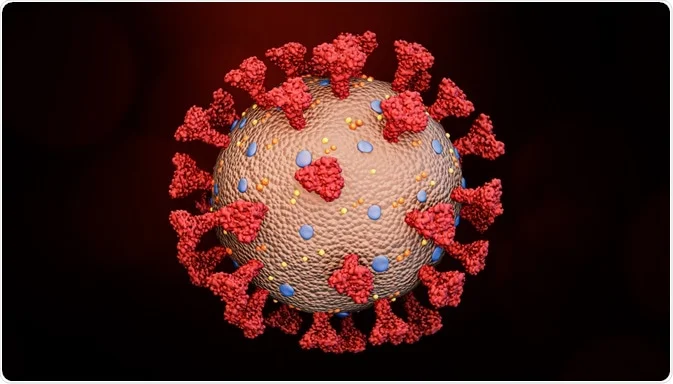
The SARS-CoV-2 and MRNA COVID-19 vaccine spike protein can directly bind to and activate mast cells, causing them to degranulate and release inflammatory mediators even after the acute infection has resolved.
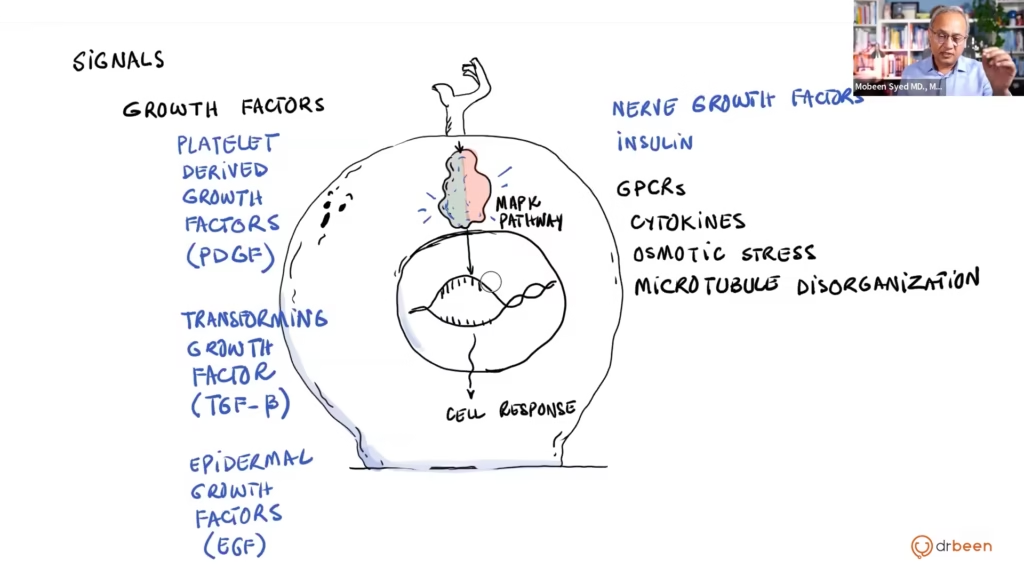
2. Immune System Dysregulation
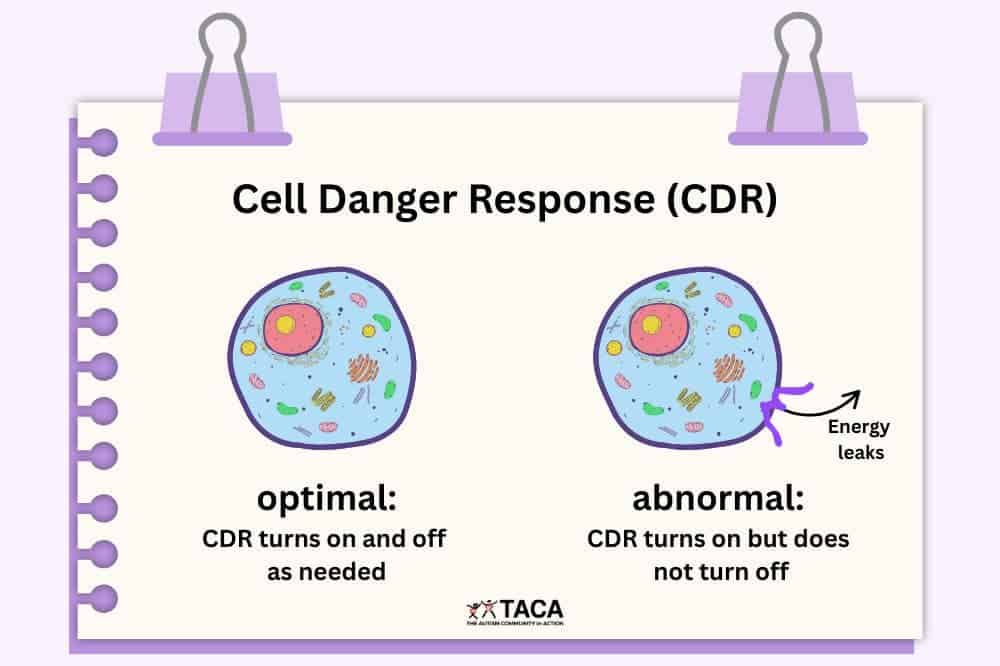
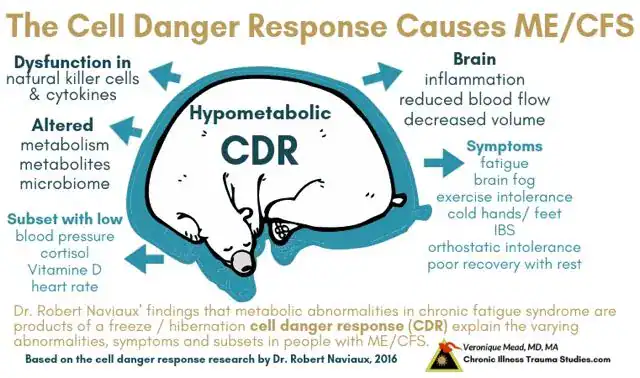
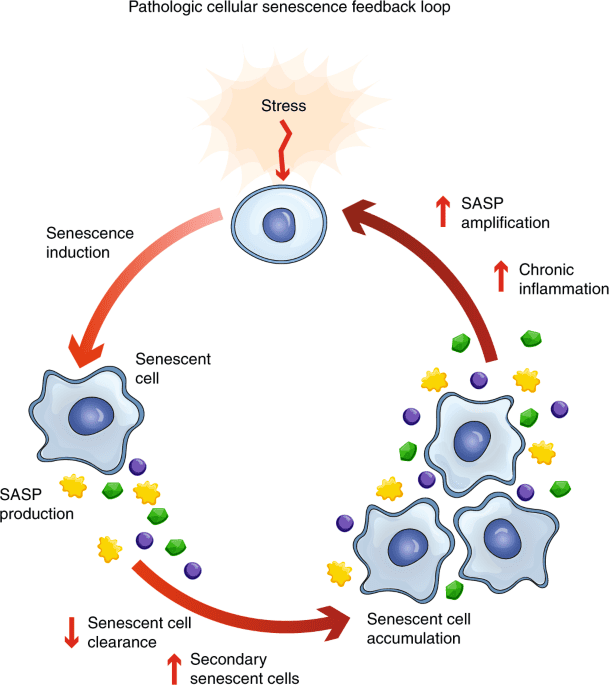
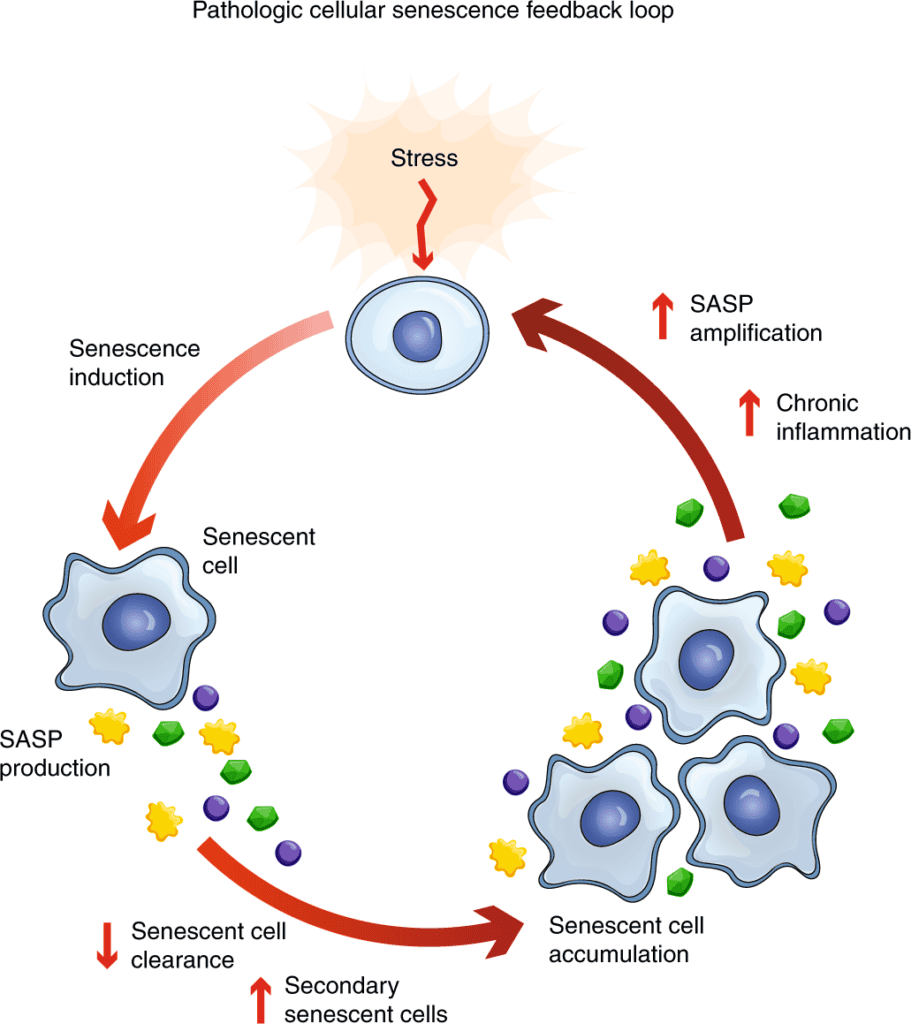
COVID-19 and mRNA COVID-19 vaccine spike protein can dysregulate the immune system, leaving mast cells in a hyperreactive state. This persistent immune activation continues long after viral clearance.
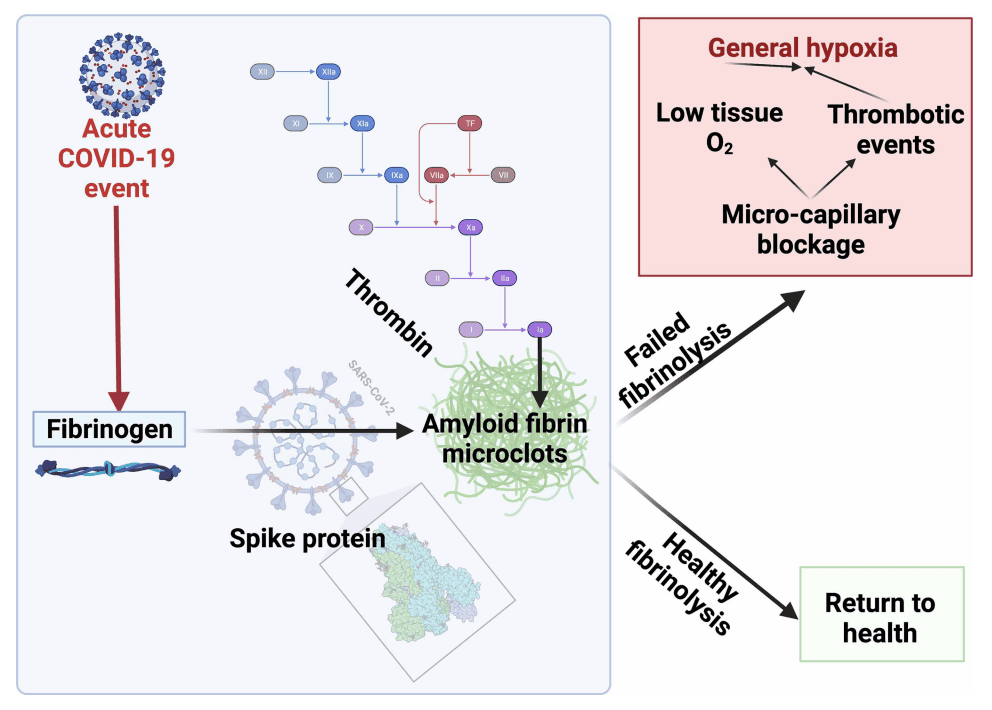
3. Microclot Formation
Emerging research shows that microclots and endothelial dysfunction in Long Covid and Post-Vaccine Syndrome may trigger mast cell activation as part of the inflammatory response.
4. Autonomic Dysfunction
POTS (Postural Orthostatic Tachycardia Syndrome) and other forms of dysautonomia common in Long Covid and Post-Vaccine Syndrome can trigger mast cell degranulation, creating a vicious cycle.
5. Persistent Spike Protein
Studies suggest spike protein may persist in tissues for months after infection or vaccination, providing ongoing stimulation to mast cells.
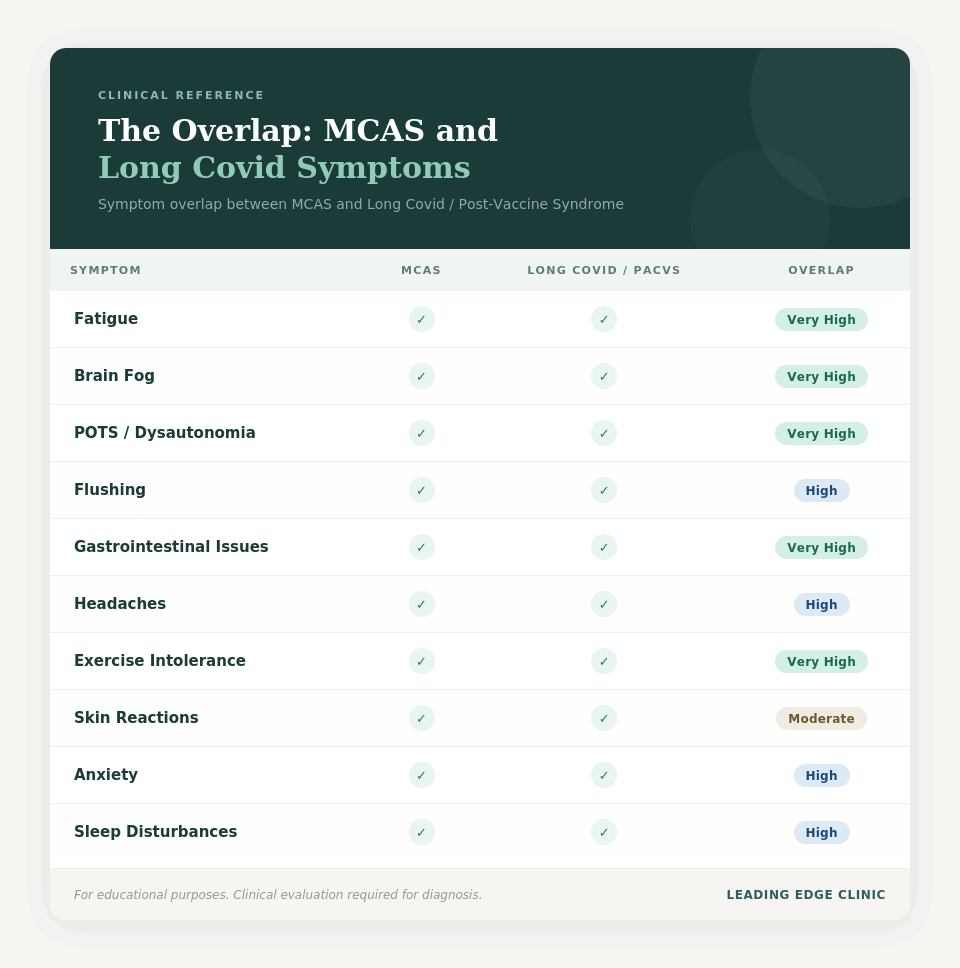
The Overlap: MCAS and Long Covid Symptoms
The symptom overlap between MCAS and Long Covid/Post-Vaccine Syndrome is striking:
| Symptom | MCAS | Long Covid/Post-Vaccine Syndrome | Overlap |
| Fatigue | ✓ | ✓ | Very High |
| Brain Fog | ✓ | ✓ | Very High |
| POTS/Dysautonomia | ✓ | ✓ | Very High |
| Flushing | ✓ | ✓ | High |
| Gastrointestinal Issues | ✓ | ✓ | Very High |
| Headaches | ✓ | ✓ | High |
| Exercise Intolerance | ✓ | ✓ | Very High |
| Skin Reactions | ✓ | ✓ | Moderate |
| Anxiety | ✓ | ✓ | High |
| Sleep Disturbances | ✓ | ✓ | High |
This overlap makes MCAS treatment a crucial component of Long Covid and Post-Vaccine Syndrome care.
____
MCAS Symptoms in Long Covid Patients
MCAS in the context of Long Covid and Post-Vaccine Syndrome presents with a constellation of symptoms that can be confusing and debilitating. Understanding these symptoms is the first step toward proper diagnosis and treatment.
Common MCAS Symptoms in Long Covid:
Cardiovascular Symptoms:
- Rapid heart rate (tachycardia), especially upon standing
- Blood pressure fluctuations (both high and low)
- Palpitations
- Chest discomfort or pain
- Flushing episodes (face, neck, chest)
- Temperature dysregulation
- Endothelial dysfunction and inflammation
Gastrointestinal Symptoms:
- Nausea and vomiting
- Abdominal pain or cramping
- Diarrhea or constipation (or alternating)
- Bloating and distension
- Food intolerances (new or worsening)
- Reflux and heartburn
Neurological Symptoms:
- Brain fog and cognitive dysfunction
- Difficulty concentrating
- Memory problems
- Headaches or migraines
- Dizziness and lightheadedness
- Tingling or numbness (peripheral neuropathy)
- Anxiety and panic attacks
Dermatological Symptoms:
- Hives (urticaria)
- Itching without visible rash
- Flushing
- Skin sensitivity
- Easy bruising
- Rashes
Respiratory Symptoms:
- Shortness of breath
- Wheezing
- Throat tightness or swelling sensation
- Nasal congestion
- Post-nasal drip
Musculoskeletal Symptoms:
- Joint pain
- Muscle aches
- Bone pain
- Generalized body aches
Systemic Symptoms:
- Severe fatigue
- Post-exertional malaise (PEM)
- Exercise intolerance
- Sleep disturbances
- Temperature sensitivity
- Chemical sensitivities
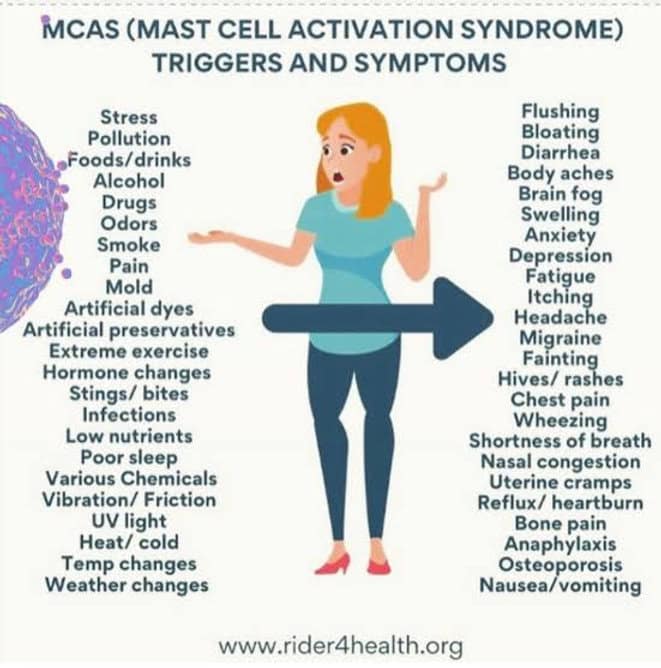
Triggers Common in Long Covid MCAS:
Understanding your triggers is essential for managing MCAS. Common triggers include:
Environmental:
- Temperature changes (especially heat)
- Strong scents or fragrances
- Chemicals and cleaning products
- Air pollution
- Mold exposure
Dietary:
- High-histamine foods (aged cheese, fermented foods, alcohol)
- Histamine-releasing foods (citrus, tomatoes, strawberries)
- Food additives and preservatives
- Processed foods
Physical:
- Exercise or physical exertion
- Stress (physical or emotional)
- Sleep deprivation
- Infections
- Menstrual cycle changes
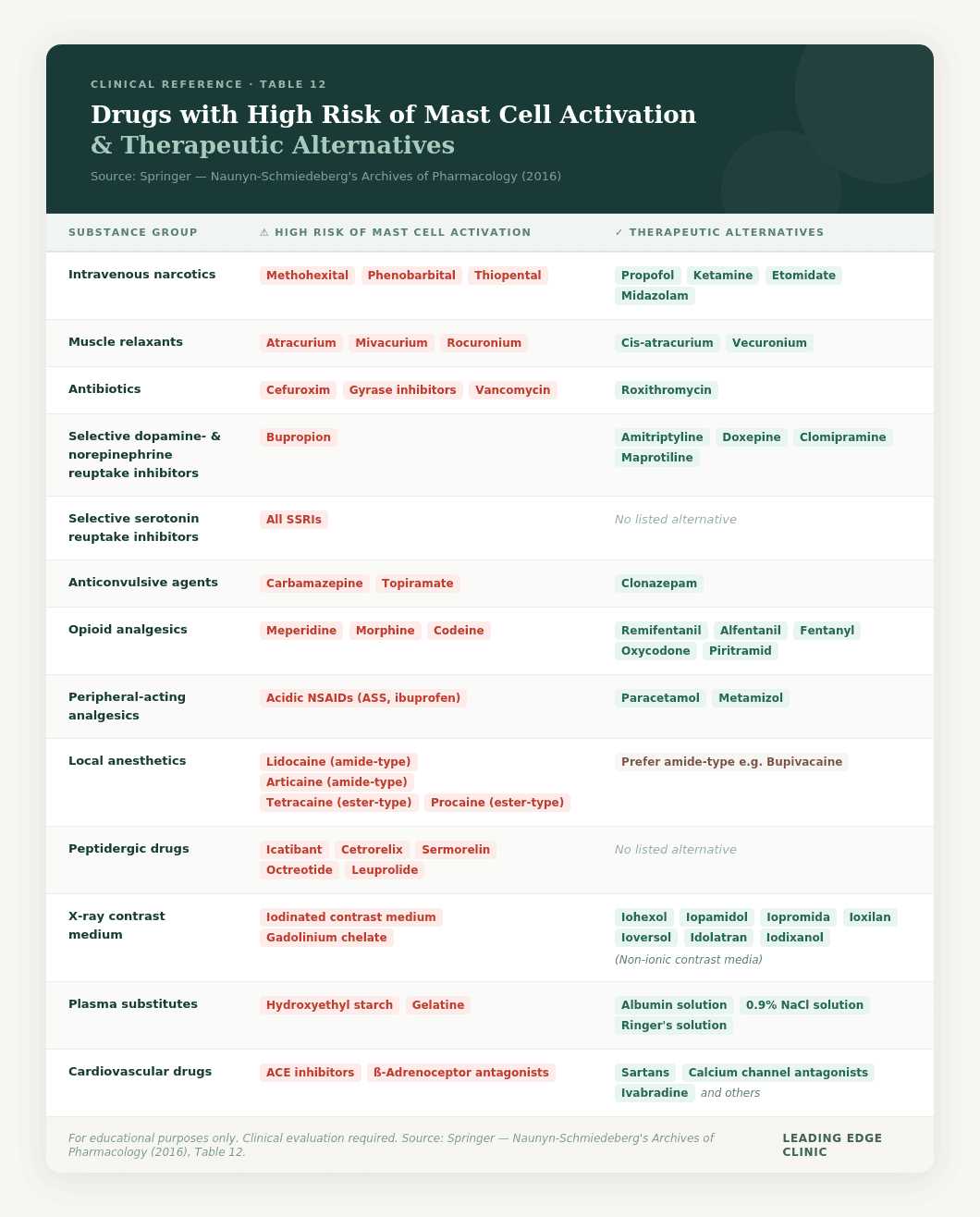
Medications:
- NSAIDs (ibuprofen, aspirin)
- Opioids
- Some antibiotics
- Reference Table 12
- Contrast dyes
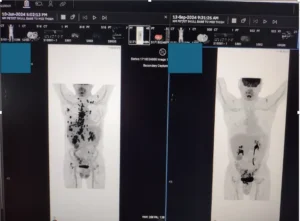
The last one is tricky and represents some of the challenging clinical judgments we must make. For example, Iliac Venous Compressions is a common condition seen in our Long Haul Covid and Post-Vaccine Syndrome patients. The endothelial dysfunction and inflammation leads to anatomically predisposed patients to developing common left iliac compressions that greatly reduce venous return flow. It is a double-edge sword because venous insufficiency and blood pooling then worsen MCAS.
To diagnose Iliac Venous Compression, patients must receive a specialized MR-Venogram protocol developed by our colleague and IVC expert, Dr. Brooke Spencer. This requires gaddolinium-based contrast agents, which do not come without risk. However, in many cases, the potential benefit of identifying and treating an Iliac Venous Compression may greatly outweight the risk of the contrast dye. There are also steps that can be taken to prevent MCAS reactions.
____
How MCAS is Diagnosed
Diagnosing MCAS, especially in the context of Long Covid and Post-Vaccine Syndrome, can be challenging. There’s no single definitive test, and diagnosis typically requires a combination of clinical evaluation and laboratory findings.
Diagnostic Criteria
According to consensus criteria, MCAS diagnosis requires:
1. Clinical Symptoms
- Recurrent or chronic symptoms involving at least 2 organ systems
- Symptoms consistent with mast cell mediator release
2. Laboratory Evidence
- Elevated tryptase, histamine, or other mast cell mediators during symptomatic episodes
- OR elevation of 20% above baseline tryptase
3. Response to Treatment
- Improvement with mast cell stabilizers, antihistamines, or other MCAS-directed therapy
Often, we only use criteria 1. and 3. because it is the most clinically and financially efficient way to help patients.
Laboratory Tests for MCAS:
During a Flare (Symptomatic Testing):
These tests are most useful when done during active symptoms:
- Serum Tryptase – Most reliable MCAS marker
- 24-hour Urine Tests:
- N-methylhistamine
- Prostaglandin D2 (PGD2)
- Leukotriene E4
- Plasma Histamine (difficult to measure accurately)
- Chromogranin A
Baseline Testing:
- Baseline Serum Tryptase – Establishes your personal baseline
- Complete Blood Count (CBC) – Rules out other conditions
- Comprehensive Metabolic Panel
- Vitamin D levels (often low in MCAS)
Challenges in Diagnosing MCAS in Long Covid:
- Timing Issues: Mediator levels must be checked during symptoms, which requires careful planning
- Test Availability: Not all labs offer comprehensive MCAS testing
- Overlapping Conditions: Long Covid involves multiple conditions that can mimic MCAS
- Normal Results: Some MCAS patients have normal lab values but clear clinical symptoms
Clinical Diagnosis:
At Leading Edge Clinic, we often make a clinical diagnosis of MCAS when:
- Patient has characteristic multi-system symptoms
- Symptoms are episodic and triggered
- There’s a clear temporal relationship with COVID-19 infection
- Symptoms respond to MCAS treatment
- Even if laboratory confirmation is not obtained
This pragmatic approach allows us to begin treatment without delay, which can be life-changing for patients.
____
Why MCAS Treatment Requires Specialized Clinical Care
Understanding MCAS is the first step. Treating it effectively is a different matter entirely — and one that requires experienced clinical guidance rather than self-directed protocols.
MCAS Treatment Is Highly Individualized
No two MCAS patients present identically, and more importantly, no two MCAS patients respond identically to treatment. What stabilizes one patient’s mast cells can trigger a significant flare in another. The same antihistamine that brings one patient relief can worsen symptoms in someone with a slightly different presentation or underlying trigger.
Like Long Haul Covid and Post-Vaccine Syndrome, MCAS is not a condition where a supplement list or a protocol found online translates reliably from one person to the next. The variables involved — trigger identification, mediator patterns, comorbidities like dysautonomia or microclotting, and the interaction between MCAS and other spike protein pathologies — require careful, individualized assessment before any intervention is introduced.
The Risk of Self-Directed Treatment
Many patients with Long Covid and Post-Vaccine Syndrome come to us after months or years of attempting to manage MCAS on their own, often based on protocols circulating in patient communities. A common pattern we see:
- Initial improvement followed by an unexpected flare
- Worsening of symptoms after adding supplements that are widely recommended online
- New sensitivities developing as a result of unguided interventions
- Delayed recovery because foundational issues — microclotting, viral reactivation, mitochondrial dysfunction — were never addressed alongside the MCAS
- Worst case scenario: a severe acute medical episode, such as a thrombotic event or anaphylactic event
MCAS rarely exists in isolation in spike protein-related illness. Treating it without addressing the broader clinical picture often means treating a symptom of a deeper problem rather than the problem itself. An example of potentially dangerous self-treatment might be cold therapy. Cold therapy is fantastic for stabilizing mast cells naturally. However, with Long Covid and Post-Vaccine Syndrome patients where thrombotic events are already a concern, cold therapy can potentially be dangerous due to rapid vasoconstriction and high blood pressure. Additionally, cold therapy can be an anaphylactic trigger for some MCAS patients.
What Effective MCAS Treatment Actually Involves
In the context of Long Covid and Post-Vaccine Syndrome, a structured MCAS treatment approach typically requires:
- Trigger identification before any intervention — environmental, dietary, medication-related, and pathogen-related triggers must be mapped to avoid compounding the problem
- Careful sequencing of mast cell stabilizers and antihistamines based on individual tolerance, starting low and titrating slowly
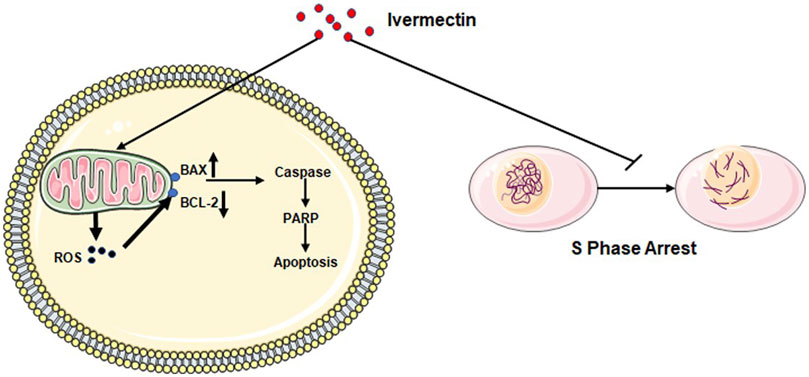
- Concurrent treatment of underlying spike protein pathology, microclotting, and immune dysregulation — because MCAS that is driven by persistent spike protein will not resolve through mast cell management alone
- Ongoing monitoring and adjustment as the patient’s overall condition changes throughout recovery
This level of personalization is not possible without a provider who understands both MCAS and the specific pathophysiology of spike protein-related illness.
____
When to Seek Specialized Care
While some MCAS symptoms can be managed with over-the-counter antihistamines and dietary changes, many Long Covid and Post-Vaccine Syndrome patients benefit from specialized care.
Signs You Need Specialized MCAS Treatment:
Severity Indicators:
- Symptoms significantly impacting daily function
- Unable to work or perform normal activities
- Multiple failed treatment attempts
- Severe reactions to multiple foods
- Anaphylaxis or near-anaphylaxis episodes
- Progressive worsening of symptoms
Important to note, in the context of Long Haul Covid and Post-Vaccine Syndrome, complex interplay of spike protein may explain failed treatment attempts. Additionally, these indicators do not include the “slow burn” of worsening and unexplained symptoms many MCAS patients face. For example, roaming pain, endothelial dysfunction, and much more. If your symptoms are listed, that doesn’t mean it is not severe.
Complexity Indicators:
- Symptoms involving 3+ organ systems
- Multiple medication sensitivities
- Coexisting conditions (POTS, ME/CFS, EDS)
- Unclear diagnosis (symptoms don’t fit typical patterns)
- Need for advanced treatments
What Specialized MCAS Care Provides:
Comprehensive Evaluation:
- Detailed symptom history
- Trigger identification
- Appropriate laboratory testing (if desired; but not necessary)
- Discussion on interplay with Long Haul Covid and PACVS
- Root cause discussion
Personalized Treatment Plans:
- Customized medication protocols
- Dietary guidance specific to your triggers
- Supplement recommendations
- Lifestyle modification strategies
Ongoing Management:
- Regular follow-up to adjust treatments
- Support during flares
- Coordination with other specialists
- Long-term monitoring and optimization
Leading Edge Clinic’s Approach:
At Leading Edge Clinic, we specialize in MCAS in the context of Long Covid and Post-Vaccine Syndrome. Our approach includes:
✅ Telemedicine Nationwide: Accessible from all 50 states
✅ Expert Providers: Deep understanding of and clinical experience treating spike-protein induced MCAS
✅ Proactive RN Follow-Up: Regular check-ins between appointments
✅ Comprehensive Protocols: Evidence-based treatment combining conventional and integrative approaches
✅ Whole-Person Care: Addressing MCAS alongside other Long Covid and PACVS symptoms and root causes
____
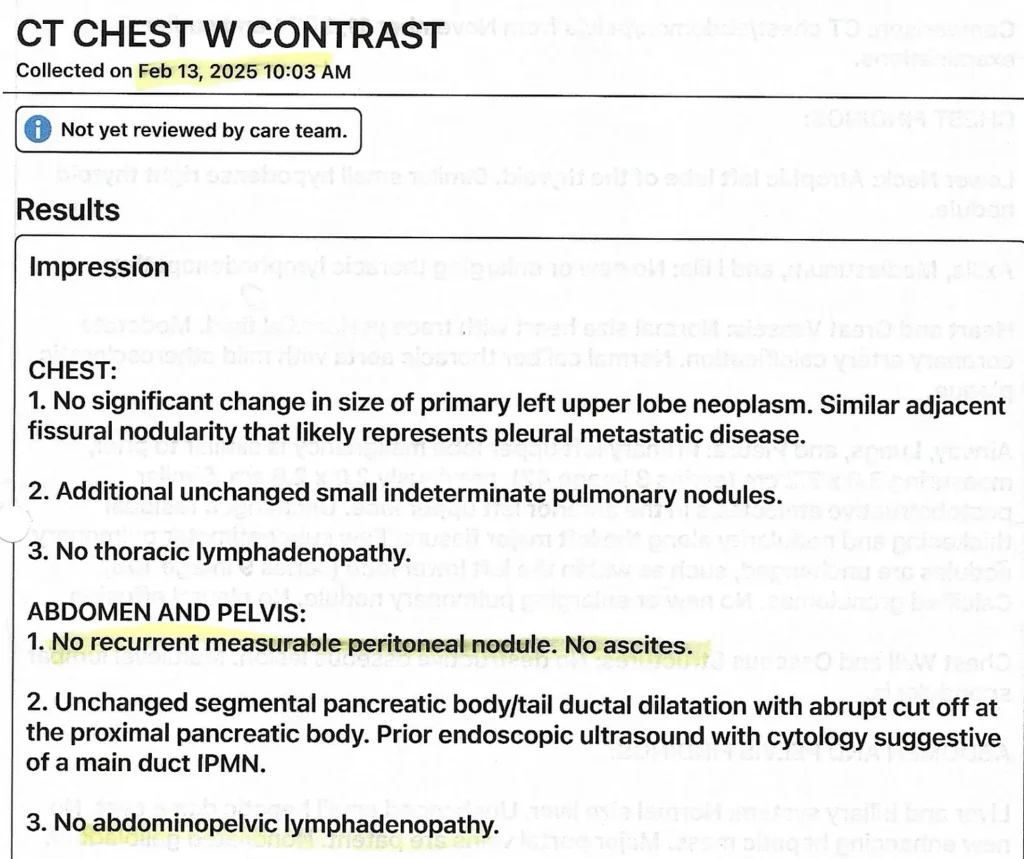
Patient Success Stories
*Names changed to protect privacy*
Sarah’s Story: From Unable to Eat, To Enjoying Her Favorite Foods
Background: 67-year-old business administrator for a local business developed Long Covid after infection in Spring 2023. By 2024, she was experiencing:
- Severe fatigue and post-exertional malaise
- Dypsnea upon exertion and at rest
- POTS with palpitations upon standing
- Multiple food intolerances; “hardly able to eat anything”
- Intolerances to self-administered treatments (supplements)
- Constant nausea and GI distress
- Severe anxiety (did not previously have)
MCAS Diagnosis: Clinical diagnosis based on multi-system symptoms and clear triggers (other issues at play with Long Covid, but focusing on MCAS for this)
Treatment Protocol:
- Experimentation with various antihistamines (H1/H2)
- Experimentation with mast cell stabilizing medications and nutraceuticals
- Low histamine diets during early healing phases
- Cold water therapy once no longer contraindicated
- Low-Dose Naltrexone used to address systemic inflammation, but also appeared to have mast cell stabilizing effect
- Other therapuetics to deal with spike protein resevoirs, microclotting, and typical Long Haul Covid issues
- Nervous system regulation program – Safe & Sound Protocol
Outcome over a year course of treatment:
- Slowly able to add in more foods; now able to consume high histamine foods like kefir and sauerkraut
- Symptom abatement enabled recreational travel
- Heart rate normalized; absence of palpitations
- Cessation of dypsnea
- Able to tolerate other therapies used for other aspects of Long Haul Covid
—
Jim’s Story: Post-Vaccine MCAS Recovery
Background: 32-year-old and high functioning; slowly developed worsening symptoms a year after COVID vaccine until bedbound
- Severe chest pain upon exertion, and eventually without exertion
- Venous insufficiency and Iliac Venous Compression
- Severe neurological symptoms
- Nausea and palpitations after eating
- Eosinophilic Esophagitis and high eosinophil count
- GERD with vomitting after meals occurring multiple times a week
- Severe and unrelenting fatigue and PEM
MCAS Diagnosis: Patient had a long list of severe symptoms, not all related to MCAS. MCAS suspected due to new onset food sensitivities and diagnosed eosinophilic esophagitis, plus consistently high eosinophil blood counts
Treatment Protocol:
- Elimination diet into carnivore diet during early treatment phases to calm histamine responses
- No response to antihistamines
- Significant clinical response to compounded Ketotifen
- Once microclots were dealt with, addition of cold exposure as tolerated
- Once weight was regained, long-term fasts to safely degranulate mast cells
Outcome: Over the course of a year and a half of treatment
- No longer bedbound; working multiple demanding jobs
- Complete cessation of GERD and vomitting
- Appropriate eosinophil levels
- Healing of gut barrier lead to improved nutrient uptake and weight regain
- Able to tolerate previously intolerable foods
- Cessation of food-induced palpitations
- Exercise tolerance improving
- Chest pain resolved
- “With the severity of my symptoms, I would go to bed every night wondering if I was going to wake up. Thanks to Scott Marsland, I got my life back and more.”
Please keep in mind these truncated success stories leave out many details relevant to the patients medical history, treatment, and recovery. These are complex, multi-system illnesses that often require the care of a knowledgeable clinician. The information in these cases is not to be interpreted as medical advice.
Frequently Asked Questions
Is MCAS permanent?
MCAS in the context of Long Covid and PACVS often improves over time with proper treatment. Many patients see significant stabilization of symptoms within their first 6 months. After addressing some of the other complexities of Long Haul and PACVS, some patients even report tolerating foods they never tolderated, even before their illness. The key is early recognition and comprehensive treatment.
How long does it take for MCAS treatment to work?
Many patients notice some improvement within 2-4 weeks of starting comprehensive treatment. Significant symptom reduction can take anywhere from weeks to months, depending on case severity. This may be further complicated by Long Haul Covid and Post-Vaccine Syndrome. Unlike many white blod cells, mast cells take years to break down. This means patients should exercise caution when reintroducing triggers, even if they are feeling better and tolerating those things well. Various therapies can speed up the process of mast cell removal.
Can I still eat my favorite foods?
Many patients find that after stabilizing their mast cells with medications, they can gradually reintroduce foods. The strict low-histamine diet is often temporary, after which you can carefully test tolerance to individual foods.
Do I need to see an allergist or immunologist?
While allergists and immunologists can be helpful, many are not familiar with MCAS, especially in the Long Covid context. You need a provider experienced with MCAS and Long Covid specifically. This may be a Long Covid specialist, integrative medicine physician, or functional medicine practitioner.
Can children develop MCAS from Long Covid?
Yes, children can develop MCAS as part of Long Covid or post-vaccine syndrome. Symptoms and treatment are similar, though dosing is adjusted for age and weight.
Is MCAS the same as having allergies?
No. While both involve histamine and mast cells, they’re different conditions:
- Allergies: Specific triggers (peanuts, pollen), IgE-mediated, predictable reactions
- MCAS: Multiple triggers, not always IgE-mediated, variable reactions
MCAS patients can have symptoms without any specific allergen exposure.
What’s the difference between MCAS and histamine intolerance?
Histamine Intolerance: Inability to break down dietary histamine properly (often due to DAO deficiency)
MCAS: Excessive production of histamine by overactive mast cells
Many Long Covid patients have BOTH conditions, which is why treatment addresses both dietary histamine AND mast cell activation.
Can stress trigger MCAS flares?
Absolutely. Stress is one of the most common MCAS triggers. Stress hormones can activate mast cells directly. This is why stress management is a crucial part of MCAS treatment. We recommend the Safe & Sound Program f0r autonomic nervous system regulation.
Should I avoid all histamine-releasing foods forever?
No. The goal is to stabilize mast cells with medications, then gradually expand your diet. Most patients can eventually tolerate moderate amounts of higher-histamine foods, especially when mast cells are well-controlled with treatment.
Can MCAS cause anxiety and depression?
Yes. Histamine and other mast cell mediators directly affect the brain and can cause:
- Anxiety and panic
- Depression
- Brain fog
- Insomnia
- Mood swings
Many patients find that treating MCAS improves their mental health significantly.
Next Steps: Getting Treatment for MCAS and Long Covid
If you recognize yourself in these symptoms, you don’t have to suffer alone. MCAS in Long Covid and Post-Vaccine Syndrome is treatable, and most patients experience significant improvement with proper care.
How to Get Started:
1. Document Your Symptoms
- Keep a symptom diary for 1-2 weeks
- Note triggers (foods, stress, temperature, etc.)
- Track timing and severity
- This helps your provider understand your patterns
2. Schedule a Consultation
At Leading Edge Clinic, we offer comprehensive evaluations for Long Covid and MCAS:
- Initial telemedicine consultation with experienced provider
- Personalized treatment plan
- Ongoing support with proactive RN follow-up
- Available in all 50 states
3. Implement Basic Strategies
While waiting for your appointment, you can start:
- Begin reducing high-histamine foods
- Keep detailed food and symptom diary
4. Gather Your Medical Records
- Previous COVID test results
- Recent lab work
- Current medications
- Prior treatments attempted
Why Choose Leading Edge Clinic for MCAS Treatment?
✅ Specialized Expertise: Our team has treated thousands of Long Covid and Post-Vaccine Syndrome patients, many presenting with MCAS
✅ Comprehensive Approach: We address MCAS alongside POTS, ME/CFS, microclotting, cell danger responses, systemic inflammation, and other Long Covid and Post-Vaccine Syndrome conditions
✅ Evidence-Based Protocols: Treatment based on research, pathophysiological knowledge, and clinical experience
✅ Nationwide Access: Telemedicine available in all 50 states
✅ Proactive Support: RN follow-up between appointments (unique to our practice)
✅ Compassionate Care: We understand the complexity and impact of these conditions
—
Conclusion
MCAS is a common and often overlooked component of Long Covid and Post-Vaccine Syndrome that can cause significant suffering. The good news is that with proper recognition and treatment, most patients experience meaningful improvement in their quality of life.
If you’re struggling with multi-system symptoms after COVID-19 or vaccination, MCAS may be part of the picture. Don’t wait—early intervention leads to better outcomes.
Ready to Start Your Healing Journey?
—
Resources:
– Leading Edge Clinic Patient Testimonials
– Dr. Kory’s Medical Musings Substack
– Scott Marsland’s Lightning Bug Substack
—
References
1. Afrin LB, et al. “Mast cell activation disease: An underappreciated cause of neurologic and psychiatric symptoms and diseases.” Brain Behav Immun. 2015.
2. Weinstock LB, et al. “Mast cell activation syndrome: A primer for the gastroenterologist.” Dig Dis Sci. 2021.
3. Theoharides TC, et al. “Could SARS-CoV-2 Spike Protein Be Responsible for Long-COVID Syndrome?” Mol Neurobiol. 2022.
4. Kempuraj D, et al. “COVID-19, Mast Cells, Cytokine Storm, Psychological Stress, and Neuroinflammation.” Neuroscientist. 2020.
5. Molderings GJ, et al. “Mast cell activation disease: a concise practical guide for diagnostic workup and therapeutic options.” J Hematol Oncol. 2011.
—
**Medical Disclaimer:** This article is for educational purposes only and does not constitute medical advice. Always consult with a qualified healthcare provider before starting any treatment protocol. MCAS treatment should be individualized and monitored by an experienced practitioner.