Post-Vaccine Syndrome Treatment: Why Most Approaches Fail (And What Actually Works in 2026)
If you’ve been dealing with Post-Vaccine Syndrome for months or even years at this point, you’ve probably already tried a bunch of different treatments. Your medicine cabinet may even be filled with half empty bottles of different supplements.
Maybe you worked through supplement stacks you found in Facebook groups. Maybe you were prescribed antihistamines and told you to “just rest more.” Or you dropped thousands on a functional medicine doc who ran every lab under the sun, handed you a protocol with 30 supplements, and… nothing really changed.
Here’s what we’ve learned after treating over 3,500 patients since 2022:
Most treatments don’t fail because they’re garbage. They may fail for a number of reasons. For instance, treating symptoms instead of fixing what’s actually broken. Most likely, they are failing to sequentially pick up apart the complex multi-system root issues happening with Post-Vaccine Syndrome. It’s like taking Tylenol for a broken bone. Sure, the pain might ease up temporarily, but you still have a broken bone.
In this guide, we are going to walk you through:
- Why 70%+ of PVS treatments fail
- The 7 biological mechanisms that need to be addressed for real recovery
- Why expensive testing usually doesn’t help (and often wastes your money)
- What effective treatment actually looks like
- How to spot if you’re getting proper care
This isn’t going to be a DIY protocol. PVS is way too complex for that, and honestly, we see patients regularly who’ve made themselves worse with internet treatments. Instead, I this post will focus on what GOOD treatment looks like so you can make informed decisions about your care.
Why Most Post-Vaccine Syndrome Treatments Fail
We’ve evaluated hundreds, probably thousands of patients who tried treatment elsewhere first. Here are the most common reasons their previous treatments didn’t work:
1. Single-Target Approaches
The mistake: Treating PVS like it’s one problem with one solution.
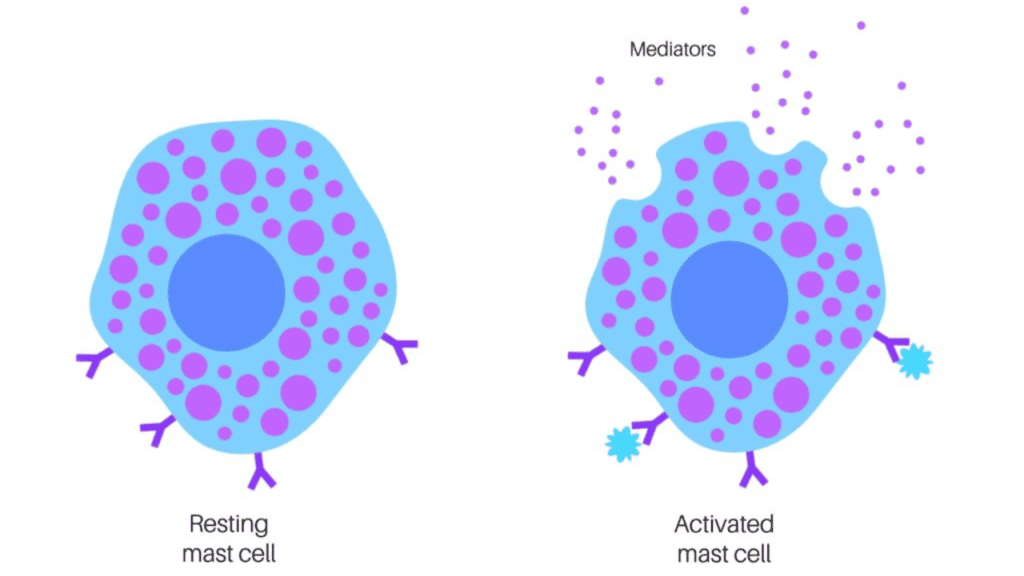
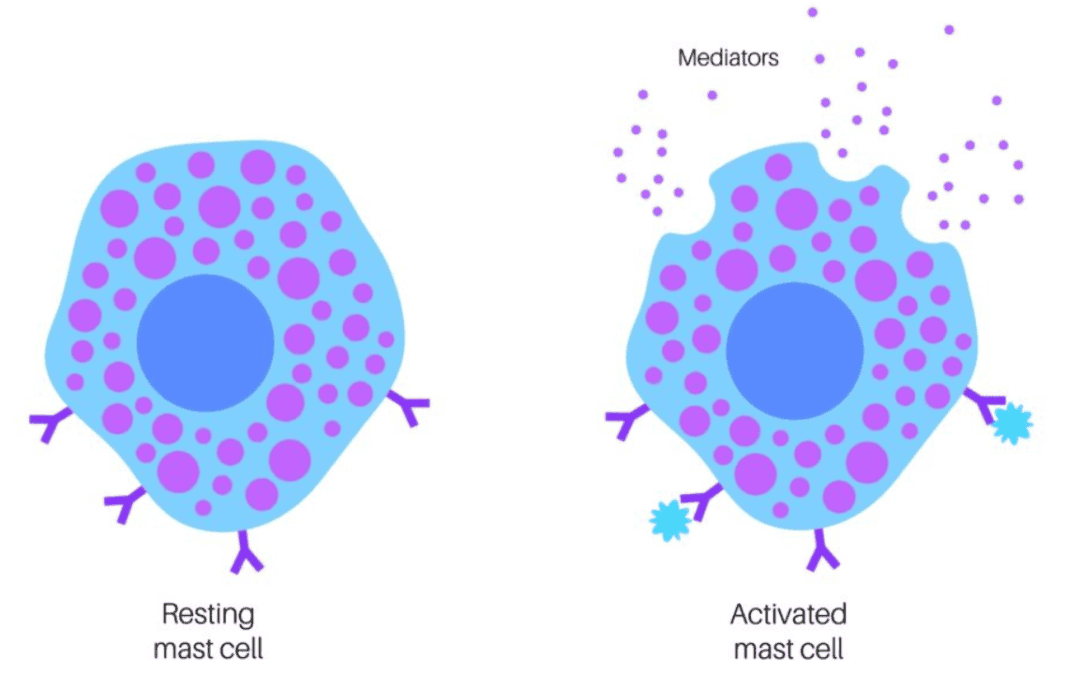
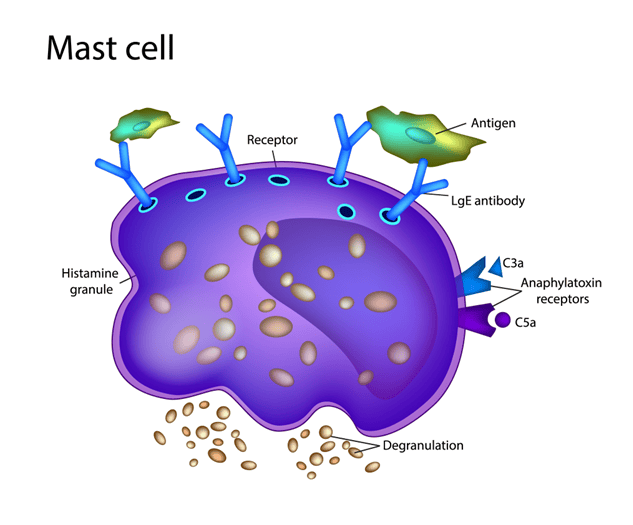
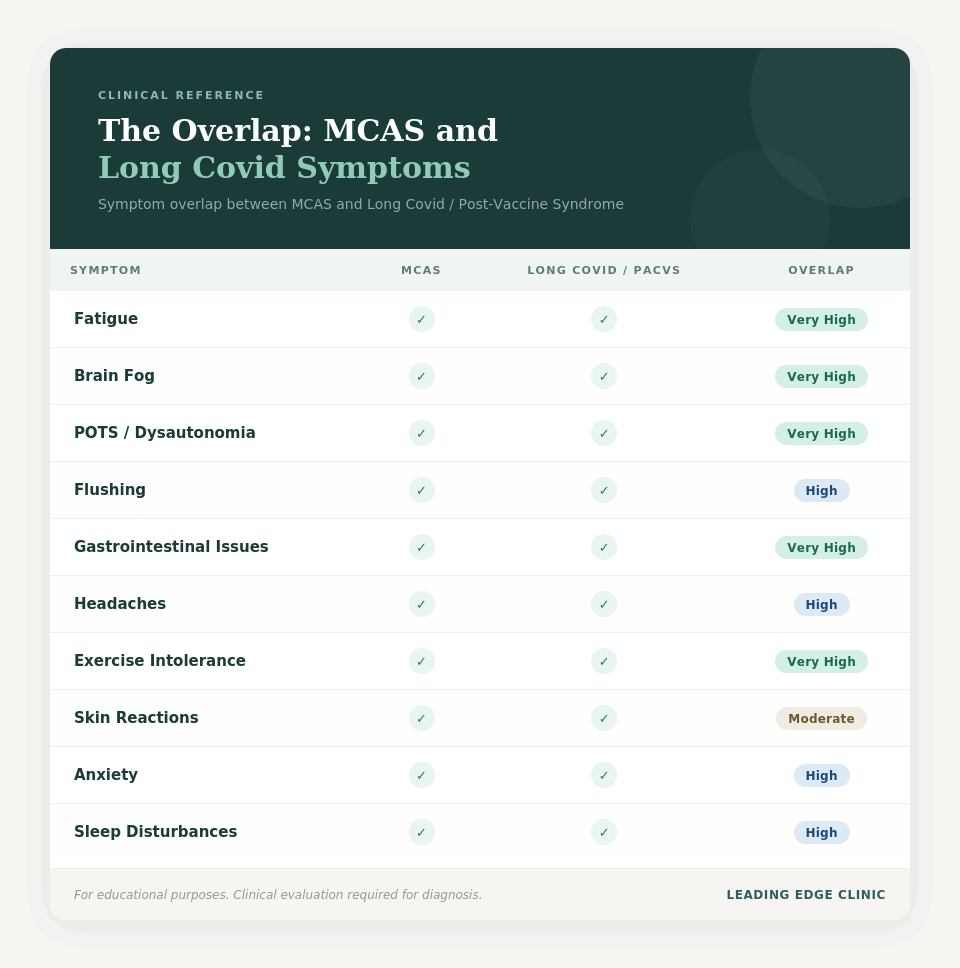
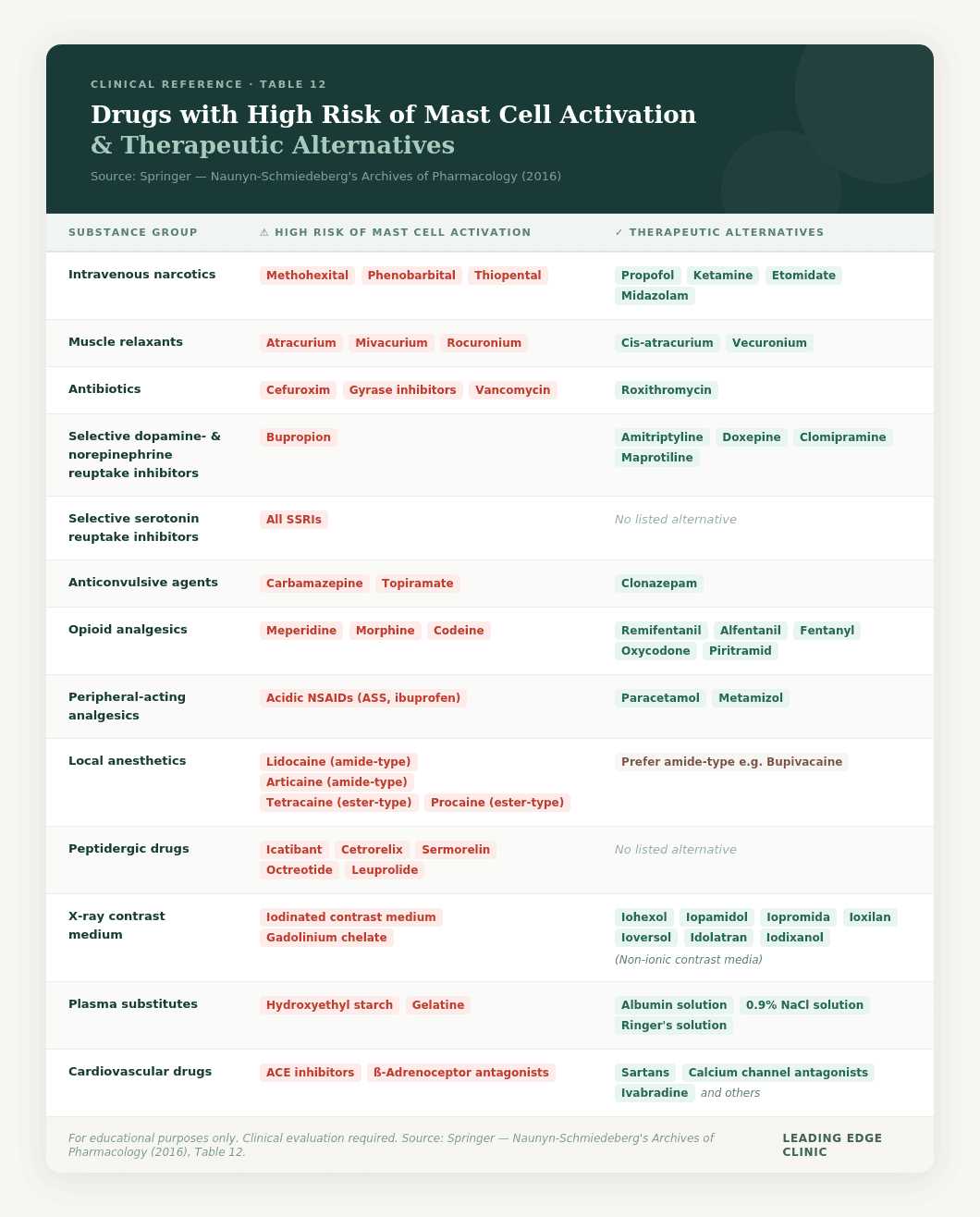
Real example: Patient comes in taking high-dose antihistamines for MCAS symptoms. Gets some relief for 2-3 weeks, then plateaus. The antihistamines are blocking one inflammatory pathway, sure. But they’re not touching the spike protein in your ACE2 receptors, your gut, or your tissue. They also aren’t addressing the microclots, the redox dysfunction, or the nervous system that’s stuck in fight-or-flight mode.
Why it fails: PVS isn’t one thing going wrong. It’s a cascade of interconnected biological dysfunctions. Fix one piece while ignoring the others? The unfixed pieces just keep perpetuating the whole mess.
What we see: Patients spend 6-12 months on single treatments, get minimal improvement, give up thinking “nothing works.”
2. Symptom Suppression Instead of Root Cause Resolution
The mistake: Making symptoms more tolerable rather than fixing what’s broken.
Real example: Patient with crushing fatigue gets prescribed stimulants or high-dose B12. This patient feels more alert for a few hours. But the underlying mitochondrial dysfunction and cellular energy crisis? Still there, getting worse. Within weeks, even the stimulants stop working.
Why it fails: If your mitochondria are damaged, your cells are stuck in emergency mode, or your cells are in a “zombie-like” senescent state, no amount of B vitamins or caffeine is going to restore actual energy. You’re basically whipping an exhausted horse.
The result: Patients become dependent on symptom suppressors that lose effectiveness over time. Meanwhile, the root causes keep getting worse.
3. The “Kitchen Sink” Approach
The mistake: Throwing 20-30 supplements at the problem without any real strategy.
Real example: Patient brings us a list of 35 supplements they’re taking. Everything from vitamin D to exotic mushroom extracts. Total monthly cost: $800. Improvement: basically none.
Why it fails: More isn’t better. Here’s what usually happens with these massive supplement stacks:
- Overlapping mechanisms (you’re triple-dosing the same pathway)
- Some contradict each other (promoting inflammation while trying to suppress it)
- Not targeting YOUR specific problems
- Wrong dosing or wrong form
- Side effects that mask whether anything’s actually working
What happens: Patients waste thousands of dollars, can’t tell what’s helping versus hurting, and often develop new symptoms from supplement interactions.
4. Chasing Lab Values Instead of Treating the Patient
The mistake: Believing expensive testing will reveal the “one thing” you need to fix.
Real example: Patient spends $5,000 on comprehensive panels. Micronutrient testing, heavy metals, genetics, specialized immune panels, food sensitivities. Gets back a 40-page report with 50 things flagged in red.
Why it fails: Here’s what we’ve learned after treating thousands of patients:
- Most PVS patients have completely normal standard labs (that’s part of why doctors dismiss them)
- A lot of specialized tests show “abnormalities” that aren’t actually relevant to PVS
- Test results often don’t change what we’d do anyway
- The most important information comes from your symptoms and how your body responds to treatment
- We already know the root causes. We don’t need $5,000 in labs to confirm them.
The reality: We’ve successfully treated thousands of patients without extensive lab work. Your money is better spent on actual treatment.
5. Stopping Treatment Too Early
The mistake: Expecting quick fixes for a complex, chronic condition.
Real example: Patient starts treatment, feels 20% better after 4 weeks, stops because they expected to be “cured” by now. Within 2-3 weeks, they’re back where they started. Or worse.
Why it fails: PVS didn’t develop overnight. It’s not going to resolve overnight either. The biological dysfunctions we’re addressing (spike protein persistence, microclots, cellular danger response, senescent cell burden) take months to fully correct.
An Example of a realistic timeline:
- Weeks 1-12: Inflammatory reduction, some symptoms improve
- Months 3-12: Steady improvement as root causes get addressed
- Year 1+: Major improvements, good days outnumber bad days
- Year 1.5+: Continued recovery, return to near-normal function
- Year 2+: Maintenance and full recovery for most patients
What we see: Patients who commit to 6-12 months of treatment? 80-85% success rate. Those who stop at 4-8 weeks? 0-5% success rate.
6. Treating PVS Like It’s Something Else
The mistake: Using protocols designed for ME/CFS, Lyme, or MCAS without modification.
Real example: Patient with PVS gets treated with a Lyme protocol. There’s overlap, absolutely. But, PVS has unique features like persistent spike protein, and significant senescent cell burden that require specific interventions. The Lyme approach misses critical pieces.
Why it fails: While PVS shares features with other post-viral conditions, it has distinct mechanisms that must be addressed. Cookie-cutter protocols from other conditions miss what makes PVS different.
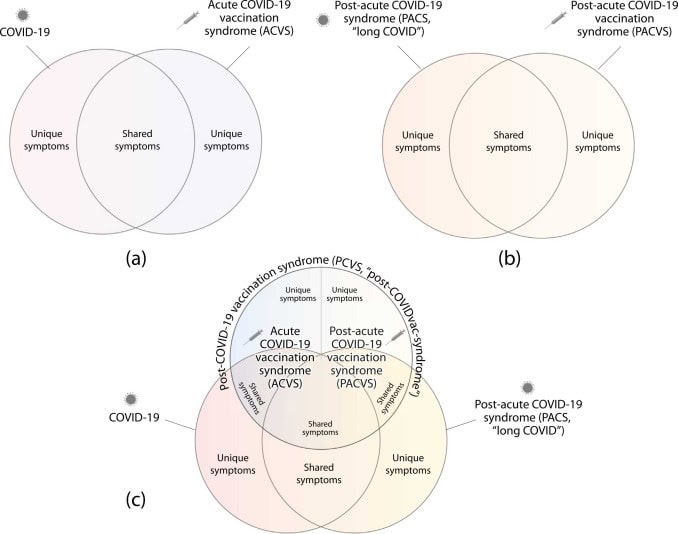
The 7 Root Causes That Must Be Addressed
After treating 3,500+ patients, we’ve repeatedly witnessed (not just read the research) seven core biological dysfunctions driving Post-Vaccine Syndrome. You need to address ALL of them. Not just one or two. And, you need to address them sequentially in a manner that makes sense.
1. Persistent Spike Protein
What’s happening: In PVS patients, vaccine-generated spike protein has been detected circulating for 6+ months. Some studies show 700+ days post-vaccination. And what about in the tissues? We know through our work with leading researchers that the spike protein uses commensal gut bacteria to hide out and act as bacteriophages. We have long known that spike protein has an affinity for ACE2 receptors to access cells. We know from post-mortem tissue staining that it is often lodged in organs and other types of tissue.
Why it matters: Spike protein isn’t just sitting there doing nothing. It’s biologically active—triggering ongoing inflammation, damaging blood vessel walls, promoting clotting, keeping your immune system in a constant state of activation, promoting a cell danger response and senescent cell signaling.
Treatment principle: Clear the persistent spike through multiple mechanisms. This isn’t a single medication. It requires a strategic combination targeting different clearance pathways.
What makes this complex:
- Spike protein “hides” in different tissues
- Clearance rate varies wildly between individuals
- Spike will alternate between gut, and systemic locations to hide out
- Some products identified for spike protein clearance can actually make the problem worse
- Different approaches depending on where spike is concentrated
- Depending on burden, can take 3-12+ months to fully clear
Why you can’t DIY this: The agents that clear spike protein also affect clotting. Too aggressive? Bleeding risk. Not aggressive enough? Persistent inflammation. Requires medical judgment and monitoring.
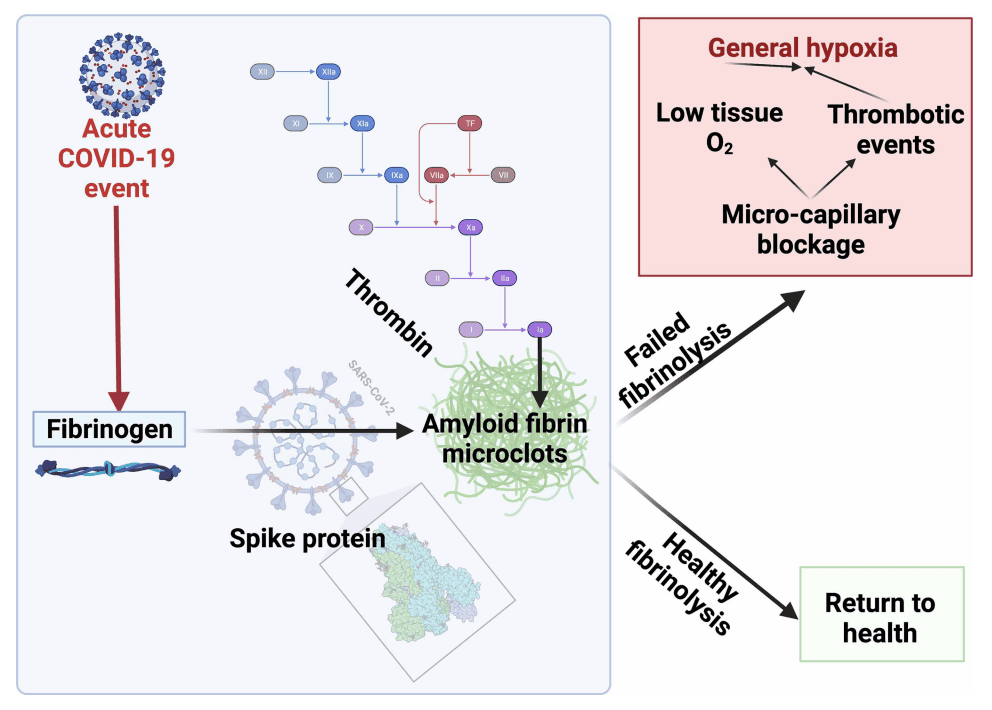
2. Microclot Formation and Vascular Dysfunction
What’s happening: Research shows PVS patients often have microclots. Tiny clots that don’t show up on standard imaging but block blood flow in small vessels. This reduces oxygen delivery to tissues. Result? Fatigue, brain fog, exercise intolerance, and more.
Why it matters: Your cells can’t function without oxygen and nutrients. Microclots create chronic tissue hypoxia (low oxygen), which perpetuates all the other dysfunctions.
Treatment principle: Break up existing microclots, prevent new formation, restore healthy endothelial function.
What makes this complex:
- Must assess bleeding risk (some patients can’t tolerate aggressive clot-busting)
- Different agents target different clot components
- Has to be coordinated with spike protein clearance (they’re related)
- Endothelial repair takes months
- Over-aggressive treatment causes its own problems (just like over-aggressive spike clearance)
Why you can’t DIY this: Anticoagulation and clot-busting agents are powerful. This needs medical supervision.
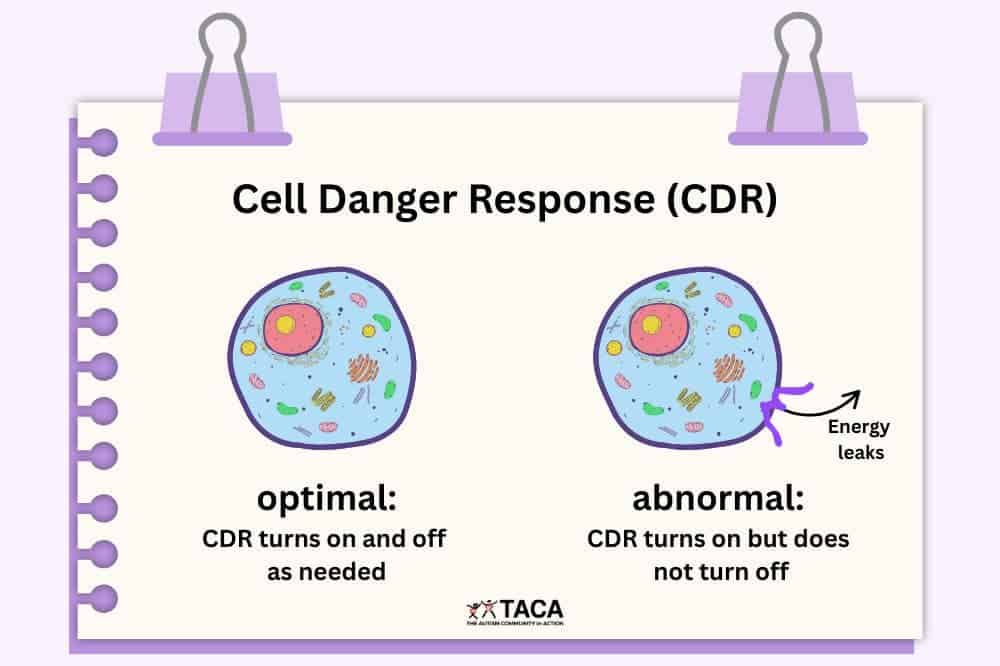
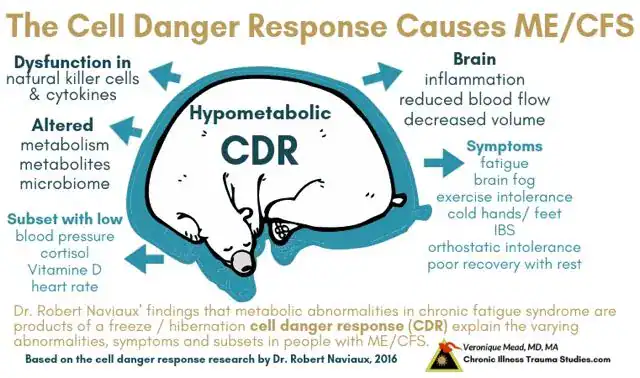
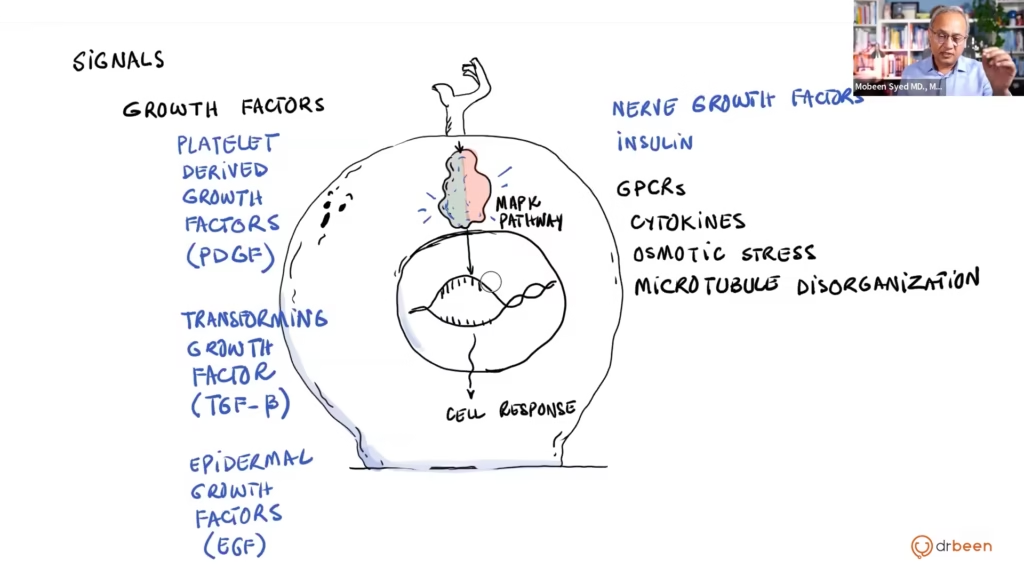
3. Chronic Cell Danger Response (CDR)
What’s happening: When cells sense a threat, they enter a protective “cell danger response.” They shut down normal functions, stop making energy efficiently, focus on survival. In PVS, cells get STUCK in this state even after the threat is gone.
Why it matters: Cells in CDR can’t do their jobs. Muscle cells can’t contract efficiently (hello, exercise intolerance). Brain cells can’t communicate well (brain fog). Immune cells malfunction. It’s like your whole body stuck in permanent emergency mode. Or, “battery saver” mode.
Treatment principle: Signal to cells that it’s safe to exit emergency mode and return to normal function. This involves addressing inflammation, restoring cellular energy production, calming danger signals.
What makes this complex:
- CDR is protective. You can’t just “turn it off”
- Requires creating conditions where cells feel safe to exit
- Different tissue types respond to different signals
- Must be addressed systematically
- Takes time. Cells don’t trust the “all clear” signal immediately
Why you can’t DIY this: Exiting CDR requires strategic sequencing. Push too hard too fast? Cells retreat deeper into defense mode. Requires clinical experience.
4. Redox Imbalance and Oxidative Stress
What’s happening: Your cells use controlled oxidation to generate energy and fight infections. But in PVS, the redox system gets thrown out of balance. Too much oxidative stress, not enough antioxidant capacity. Cells are essentially rusting from the inside.
Why it matters: Excessive oxidative stress damages mitochondria (your cellular power plants), creates inflammation, damages DNA, impairs every cellular process. It’s a major driver of fatigue, brain fog, and tissue damage.
Treatment principle: Restore redox balance. Not by flooding the system with antioxidants (which often doesn’t work), but by repairing the cellular mechanisms that regulate oxidation and reduction.
What makes this complex:
- Too many antioxidants can actually make things worse (yes, really)
- Different tissues need different redox approaches
- Must support mitochondrial function simultaneously
- Redox dysfunction and CDR feed into each other—must address both
- Requires specific nutrients and cofactors in precise forms
Why you can’t DIY this: The supplement industry sells “antioxidants” as a cure-all. In reality, crude antioxidant supplementation often fails in PVS because it doesn’t address the underlying regulatory dysfunction. Can even cause harm by disrupting what little redox balance remains.
5. Autonomic Nervous System Dysregulation
What’s happening: Your autonomic nervous system (ANS) controls automatic functions like heart rate, blood pressure, digestion, temperature regulation. In PVS, the ANS gets stuck in “fight or flight” mode or swings wildly between sympathetic and parasympathetic states.
Why it matters: ANS dysfunction causes POTS, blood pressure instability, temperature problems, digestive issues, and worsens every other symptom. Plus it’s self-perpetuating—ANS dysfunction increases inflammation and oxidative stress, which worsens ANS dysfunction.
Treatment principle: Calm the nervous system, restore autonomic balance, retrain the ANS to function normally. This involves both top-down (nervous system) and bottom-up (reducing inflammatory signals) approaches.
What makes this complex:
- ANS dysfunction has multiple causes in PVS (inflammation, redox dysfunction, microclots affecting brain blood flow, vagus nerve damage)
- Must address root causes while providing symptomatic support
- Different patients need sympathetic suppression versus parasympathetic activation
- Timing matters. Push ANS retraining too hard and symptoms worsen
- Requires months of consistent intervention
Why you can’t DIY this: Many patients try beta-blockers or other meds for POTS and get minimal relief. Why? Because they’re not addressing WHY the ANS is malfunctioning. Effective treatment requires understanding how ANS interacts with the other six dysfunctions.
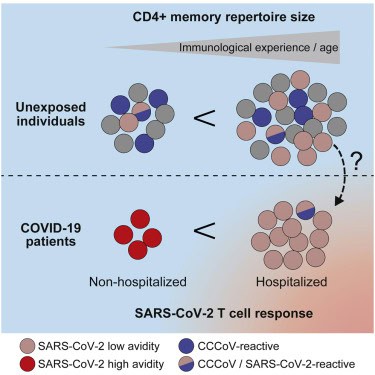
6. Immune Dysregulation
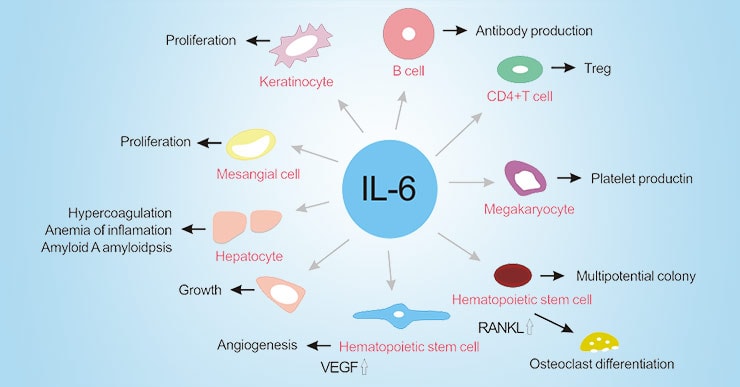
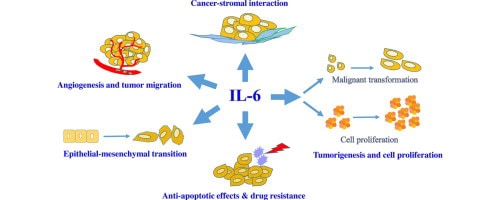
What’s happening: Healthy immune function recognizes threats, mounts appropriate response, returns to baseline. In PVS? The immune system becomes chronically dysregulated. It’s simultaneously overactive (attacking your own tissues) and underactive (failing to clear threats properly). Elevated inflammatory cytokines like IL-6 and IL-8, autoantibody formation, T-cell exhaustion, impaired immune surveillance.
Why it matters: Immune dysregulation perpetuates inflammation even after the initial trigger (vaccination) is long gone. It drives tissue damage, prevents healing, worsens fatigue, creates a vicious cycle where the immune system itself becomes part of the problem. This is also why some PVS patients develop new autoimmune symptoms or reactivation of latent viruses like EBV or HHV-6.
Treatment principle: Rebalance immune function. Not by simply suppressing it (creates other problems) or stimulating it (can worsen autoimmunity), but by restoring normal immune regulation. This involves reducing inappropriate inflammatory responses while supporting proper immune surveillance and tolerance.
What makes this complex:
- The immune system has multiple arms (innate, adaptive, cellular, humoral) that can be dysregulated in different ways
- Some patients need immune modulation, others need support, many need both
- Autoantibodies may be targeting specific receptors (adrenergic, muscarinic, etc.) requiring targeted approaches
- Timing matters—aggressive immune intervention too early can worsen inflammation
- Must address other root causes simultaneously (spike protein drives immune activation, CDR affects immune cell function)
- Reactivated viruses (if present) must be addressed or immune rebalancing fails
Why you can’t DIY this: Immune modulation isn’t something you do with random supplements. We’ve seen patients get significantly worse from inappropriate immune stimulation (making autoimmunity worse) or excessive suppression (leading to infections, viral reactivation). Requires understanding which aspects of immune function are overactive versus underactive in YOUR specific case.
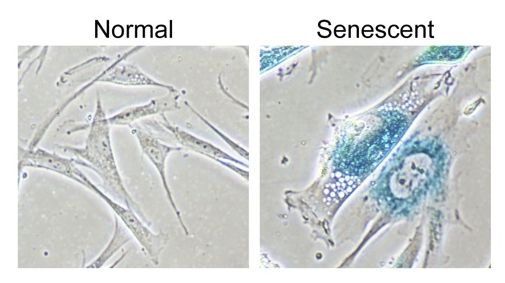
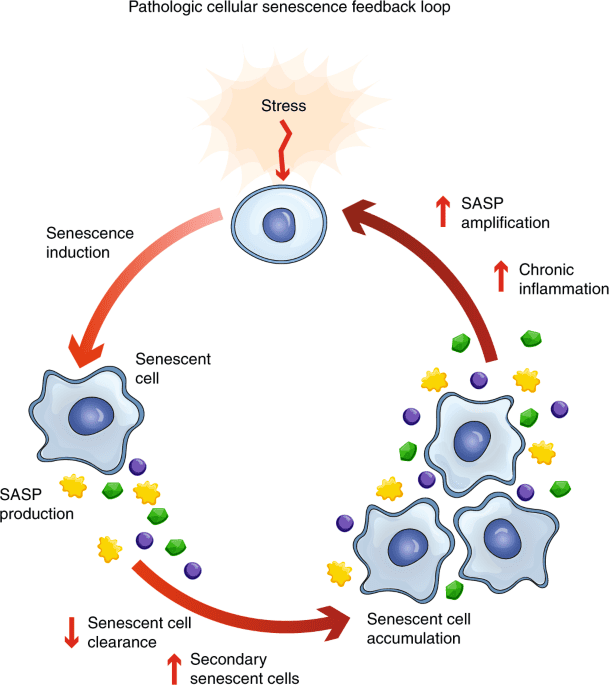
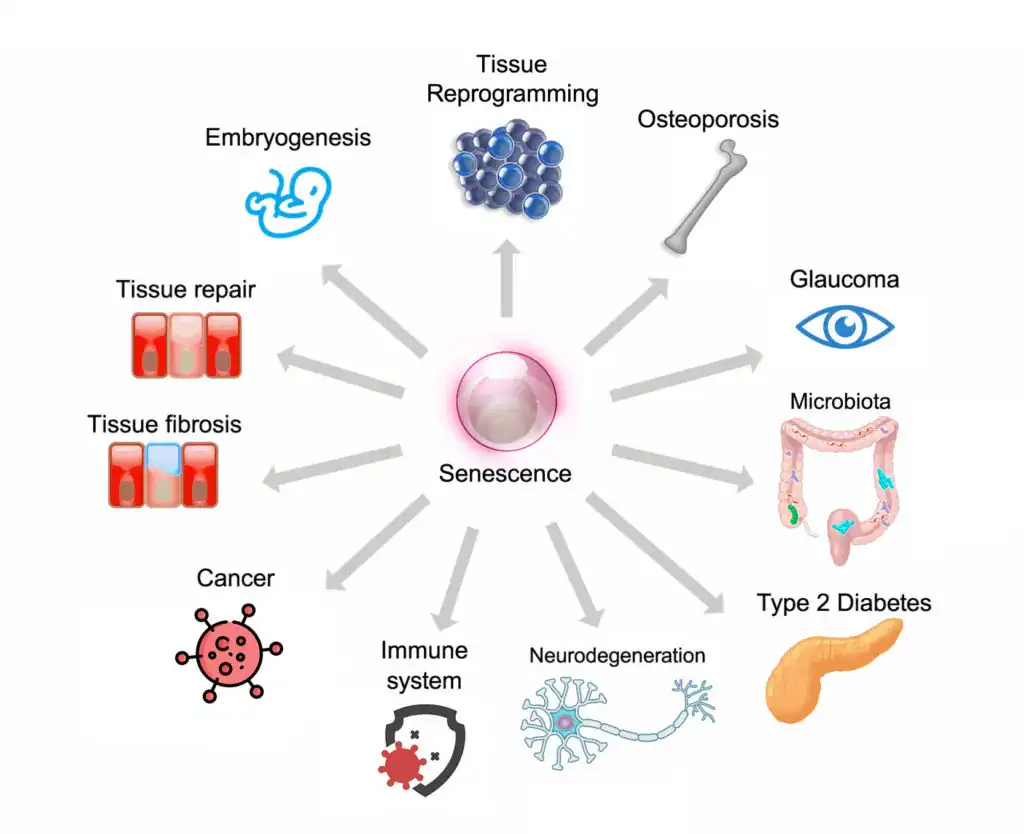
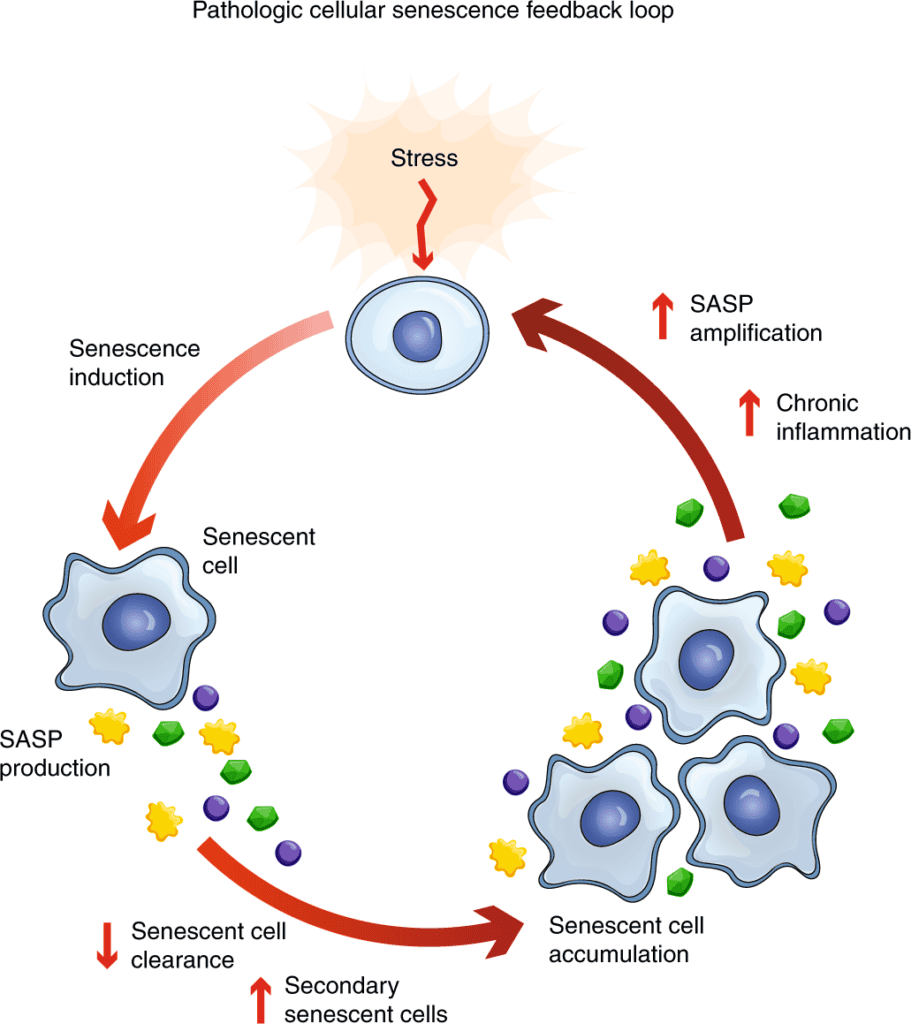
7. Senescent Cell Accumulation
What’s happening: When cells are damaged beyond repair, they’re supposed to either die (apoptosis) or get cleared by the immune system. In PVS, damaged cells often become “senescent.” They don’t die, but they don’t function either. Worse, they secrete inflammatory signals that damage surrounding healthy cells.
Why it matters: Senescent cells are zombie cells. Not alive, not dead, but toxic to everything around them. They accelerate aging, promote inflammation, prevent tissue healing. Accumulation of senescent cells is why PVS patients often feel like they “aged overnight.”
Treatment principle: Selectively eliminate senescent cells (senolysis) while preventing new senescent cell formation. This allows tissues to regenerate with healthy cells.
What makes this complex:
- Senolytics (agents that clear senescent cells) can’t be used continuously
- Must be pulsed strategically to avoid side effects
- Different senolytics target different cell types
- Timing matters—too early and too aggressive in treatment can worsen inflammation temporarily
- Must be balanced with supporting healthy cell regeneration
Why you can’t DIY this: Natural senolytics (like quercetin) get marketed heavily online, but they’re weak and often ineffective at meaningful doses. Stronger senolytics have side effects and timing considerations that require medical guidance.
Why All Seven Must Be Addressed Simultaneously
Here’s the thing: These seven dysfunctions feed into each other.
For example:
- Persistent spike protein → creates oxidative stress and inflammation → triggers immune dysregulation
- Immune dysregulation → produces inflammatory cytokines and autoantibodies
- Autoantibodies → worsen ANS dysfunction (if targeting adrenergic/muscarinic receptors)
- ANS dysfunction → increases inflammation → increased inflammation increases risk of microclotting
- Microclots → reduce oxygen delivery, worsening redox dysfunction
- Redox dysfunction → damages mitochondria and promotes CDR
- CDR → impairs immune cell function, worsening immune dysregulation
- Immune dysregulation → increases senescent cell burden
- Senescent cells → secrete inflammatory signals (SASP)
- Inflammation → worsens all other dysfunctions
- Round and round it goes.
This is why single-target treatments fail. You might temporarily suppress one piece, but the other six keep driving the system back into dysfunction.
Effective treatment has to:
- Address all seven mechanisms
- Do it in a coordinated, sequential way (not random supplements)
- Use agents that target multiple mechanisms where possible
- Be sustained long enough for the positive feedback loops to reverse
- Get adjusted based on how you respond
This is also why PVS treatment can’t be cookie-cutter. Your dominant dysfunction might be microclots and immune dysregulation. Another patient’s might be CDR and redox imbalance. Another’s might be ANS dysfunction and senescent cells. The framework is the same, but the emphasis and sequencing has to be personalized.
Why Expensive Testing Usually Isn’t Necessary
One of the most common questions: “What labs should I run before starting treatment?”
Honest answer: Probably fewer than you think.
What We’ve Learned About Testing in PVS
After treating thousands of patients:
Standard labs are usually normal in PVS
- CBC, CMP, thyroid, and inflammatory marker are either stypically unremarkable, or can jump all over the place depending on the day (highlighting the dysfunction)
- Normal labs result in conventional doctors dismissing PVS patients (“your labs are fine”)
- Normal labs don’t rule out PVS. They’re expected.
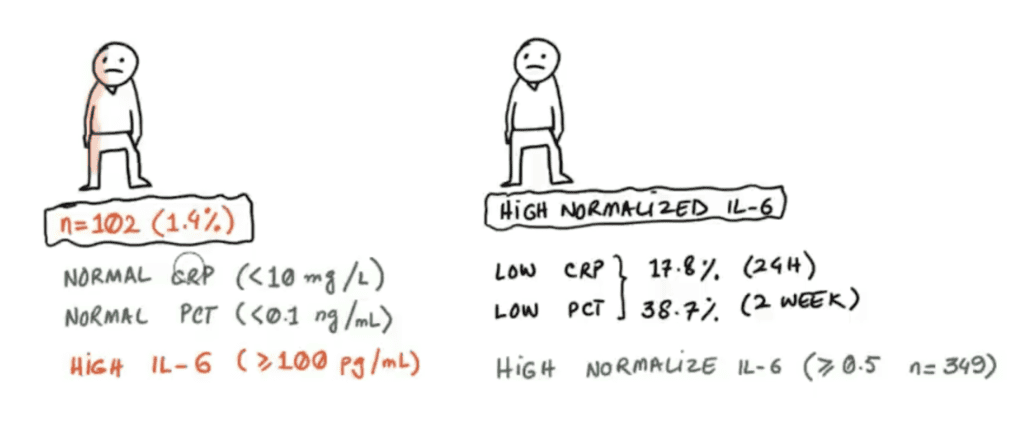
Specialized tests rarely change treatment decisions
- Yeah, we could measure your IL-6, IL-8, spike protein levels, autoantibodies
- But we already know these are likely dysregulated—you have PVS
- The treatment approach is the same whether your IL-6 is 3x or 5x elevated
- These tests cost $500-$2,000 and usually don’t alter the plan
The most important information comes from clinical evaluation
- Your symptom pattern tells us which mechanisms are dominant
- Your response to initial treatment guides adjustments
- Your exercise tolerance, POTS symptoms, cognitive function. These are your biomarkers
- We can clinically assess what’s happening without expensive labs
Testing can actually delay treatment
- Patients spend $3,000-$5,000 on comprehensive panels
- Wait 2-3 weeks for results
- Get overwhelmed by the data
- Delay starting treatment by a month or more
- That’s a month of continued suffering for information that rarely changes the plan
When We Do Recommend Testing
Look, we’re not anti-testing. We just believe testing should be strategic, not reflexive.
We might recommend basic labs if:
- You haven’t had recent standard work-up (CBC, CMP, thyroid) to rule out other stuff
- You have specific risk factors that need assessment (anemia, kidney function, etc.)
- You’re considering treatments that require baseline values
We might recommend specialized testing if:
- Your presentation is atypical and we’re considering alternative diagnoses
- You’re not responding to treatment as expected after 2-3 months
- You have insurance that covers advanced testing at no cost to you
But for most PVS patients: We know the problem. We know the root causes. We know what needs to be addressed. Let’s start treatment and see how you respond. That gives us more useful information than any lab panel.
The Money Argument
Option A: Spend $4,000 on testing
- Comprehensive panels
- Wait for results
- Start treatment 4-6 weeks later
- Treatment costs $300-500/month
- Total first 3 months: $5,900
Option B: Skip unnecessary testing
- Basic screening only ($200-400 if not covered)
- Start treatment immediately
- Adjust based on how you respond
- Treatment costs $300-500/month
- Total first 3 months: $1,600
You save $3,000-4,000 AND start treatment a month sooner.
Where would that money be better spent? On the actual treatments that make you better.
What Effective Treatment Actually Looks Like
Now that you understand what doesn’t work and what root causes must be addressed, let’s talk about what good PVS treatment actually looks like.
Note: This is NOT a DIY protocol. I’m describing the framework and principles, not specific drugs or doses. PVS treatment must be medically supervised.
The Treatment Framework
Phase 1: Foundation and Stabilization (Weeks 1-12)
Goals:
- Reduce acute inflammation
- Stabilize autonomic symptoms
- Balance redox pathways
- Gently begin spike protein clearance
- Establish baseline for monitoring progress
What happens:
- You start with a core set of interventions targeting multiple mechanisms
- Dosing is usually conservative initially to assess tolerance
- We monitor for side effects and early response
- Adjustments based on your specific symptom pattern
What to expect:
- Some patients feel worse before better (Herxheimer-like reaction from spike clearance)
- Energy might be unstable—good days and bad days
- Sleep often improves first
- Exercise tolerance usually hasn’t improved yet (too early)
- Brain fog may start to lift slightly
Phase 2: Root Cause Resolution (Months 3-9)
Goals:
- Ttirate up spike protein clearance
- Break up microclots and restore microcirculation
- Continue redox balance restoration
- Begin ently guiding cells out of danger response
- Rebalance immune function and address autoimmunity
- Gently begin clearing senescent cells (pulsed approach)
- Continue retraining autonomic nervous system through different stage
What happens:
- Treatment intensifies based on your response
- We sequence interventions strategically (some things must happen before others)
- Different mechanisms get emphasized based on what’s improving versus what’s stuck
- Monthly check-ins to assess progress and adjust
What to expect:
- Steady improvement—each month notably better than the last
- Good days start to outnumber bad days
- Exercise tolerance begins improving (slowly)
- Brain fog clears significantly
- Fatigue reduces
- Autonomic symptoms stabilize
- Occasional setbacks (normal, not linear)
Phase 3: Optimization and Maintenance (Months 9-18+)
Goals:
- Complete spike protein clearance
- Continue building mitochondrial capacity appropriately
- Begin rebuilding exercise capacity if ready
- Achieve stable autonomic function
- More aggressive senescent cell clearance and CDR therapy
- Transition to maintenance approach
What happens:
- Focus shifts from correction to optimization
- We start weaning interventions that are no longer needed
- Emphasis on supporting lasting recovery
What to expect:
- You feel like yourself again (or close)
- Energy is consistent
- Can exercise without crashes
- Brain fog is minimal to gone
- Most days feel “normal”
- Occasional mild symptoms but manageable
Key Principles of Effective Treatment
Multi-targeted, not single-agent Every intervention targets multiple dysfunctions where possible. Creates synergistic effects rather than isolated improvements.
Strategic sequencing Some interventions must come before others. Aggressively pushing mitochondrial support before addressing CDR often fails—cells won’t respond while still in danger mode. Similarly, immune modulation must be timed appropriately.
Individualized emphasis The framework is the same for all patients, but emphasis varies. If your dominant issue is POTS with adrenergic autoantibodies, we emphasize ANS, immune modulation, and microvascular interventions. We will look for an iliac venous compression to see if venous return flow is causing your POTS. If it’s crushing fatigue with immune exhaustion, we emphasize mitochondrial, redox support, and immune rebalancing.
Clinical monitoring over lab monitoring We track what matters: How’s your energy? Can you exercise? How’s your brain fog? How often do you crash? These clinical markers guide treatment better than lab values.
Patience and persistence Recovery takes 12+ months for most patients. We see the best outcomes in patients who commit to the full process rather than expecting quick fixes.
Avoiding common pitfalls We actively prevent the mistakes described earlier—no single-target approaches, no symptom suppression without addressing root causes, no premature discontinuation.
Red Flags: How to Know if You’re Getting Poor Care
Not all doctors treating PVS are equal. Here are warning signs you might not be getting good care:
Red Flag #1: They Want $5,000+ in Testing Before Starting Treatment
Why this is a problem: As discussed, extensive testing rarely changes the treatment approach. This is often more about the provider’s revenue model than medical necessity.
What good care looks like: Basic screening if needed, then start treatment. Let your response guide decisions.
Red Flag #2: They Give You a 30-Supplement Protocol on Day One
Why this is a problem: Random supplement stacks aren’t strategic. You can’t tell what’s helping, what’s hurting, what’s unnecessary. Usually based on what the provider sells.
What good care looks like: Focused, strategic approach targeting specific mechanisms. You should understand WHY you’re taking each thing.
Red Flag #3: They Promise Quick Results
Why this is a problem: Anyone promising you’ll be “cured in 4-6 weeks” doesn’t understand PVS. This is a chronic condition requiring months of treatment.
What good care looks like: Honest expectations—some improvement in 4-8 weeks, steady improvement in 3-9 months, major in 9-18+ months for most patients.
Red Flag #4: They’re Using a Cookie-Cutter Protocol
Why this is a problem: “I use the same protocol for everyone” means they’re not actually treating YOUR specific presentation.
What good care looks like: A framework that applies to all PVS patients, but with individualized emphasis and adjustments based on your specific dysfunctions and response.
Red Flag #5: They Can’t Explain the Mechanism
Why this is a problem: If your provider can’t explain WHY you’re taking something and WHAT mechanism it’s targeting, they probably don’t have a strategic framework.
What good care looks like: You should understand the treatment rationale. Good providers can explain in plain language what each intervention does and which dysfunction it addresses.
Red Flag #6: No Follow-Up or Adjustment Plan
Why this is a problem: “Call us if you have problems” isn’t a treatment plan. PVS requires regular monitoring and adjustment.
What good care looks like: Regular check-ins (usually bi-weekly in early stages), systematic assessment of progress, adjustments based on your response.
Red Flag #7: They’re Only Treating Symptoms
Why this is a problem: If all they’re offering is antihistamines for POTS, beta-blockers for heart rate, sleep aids for insomnia—they’re not addressing root causes.
What good care looks like: Symptomatic support is fine as part of comprehensive treatment, but the focus should be on resolving the underlying dysfunctions.
Why Treatment Fails Even with Good Care
Even with proper treatment, some patients don’t improve as expected. Most common reasons:
1. Ongoing Exposure or Reinjury
The problem: Continued COVID infections, additional vaccinations, or other immune triggers keep reactivating the dysfunctions you’re trying to resolve.
What happens: You improve for a few weeks, then relapse. Treatment seems to work briefly then stops. Ongoing senescent cell burden for repeat exposures is a big underlying cause
The solution: Avoiding reinjury is critical during recovery. Doesn’t mean living in a bubble, but being strategic about risk.
2. Unaddressed Comorbidities
The problem: Some patients have concurrent conditions (mold illness, Lyme, MCAS, reactivated EBV/HHV-6) that perpetuate inflammation and immune dysregulation even when PVS-specific mechanisms are addressed.
What happens: Partial improvement that plateaus around 50-60% recovery. The immune system can’t fully rebalance because there’s an ongoing trigger (chronic infection, mold exposure) keeping it activated.
The solution: Comprehensive evaluation to identify and address other contributors. For example, if you have high EBV titers from reactivation, addressing that specifically while treating PVS is essential for full recovery.
3. Non-Compliance
The problem: Missing doses, stopping and starting treatments, not following through on the full plan.
What happens: Inconsistent results, minimal improvement, frustration.
The solution: Commit to the full treatment protocol for at least 3-6 months. If cost is the barrier, discuss with your provider. There are often more affordable alternatives.
4. Unrealistic Expectations
The problem: Expecting to feel “100% cured” when you’re actually at 75-80% recovery. Or expecting linear improvement when recovery is typically wavy.
What happens: Discouragement and premature discontinuation despite actually improving.
The solution: Define what “recovery” means to you realistically. For some people, getting from 30% function to 80% function IS success, even if you’re not back to your 25-year-old peak.
The Bottom Line: What You Need to Know
If you take nothing else from this guide:
Post-Vaccine Syndrome requires addressing seven interconnected root causes
- Persistent spike protein
- Microclots and vascular dysfunction
- Chronic cell danger response
- Redox imbalance
- Autonomic nervous system dysregulation
- Immune dysregulation
- Senescent cell accumulation
Single-target treatments fail because these dysfunctions perpetuate each other You must address all seven in a strategic, coordinated way.
Expensive testing is usually unnecessary We know the root causes. Clinical evaluation and response to treatment provide better information than lab values.
Recovery takes time—usually 12+ months Anyone promising quick fixes doesn’t understand PVS. Commit to the process.
Treatment must be medically supervised This is too complex for DIY. The agents involved have real risks and require professional guidance.
Not all providers treating PVS are equal Look for someone who understands the root mechanisms, has experience treating hundreds of patients, uses a strategic framework rather than random interventions.
Most patients can recover with proper treatment Our success rate with patients who complete 9+ months of comprehensive treatment is 80-85%. This isn’t a hopeless condition.
Next Steps: Getting the Right Care
If you recognize yourself in this article—if you’ve been struggling with PVS and haven’t gotten better with other approaches—it may be time to seek specialized care.
What to Look for in a Provider
Experience matters. Look for providers who’ve treated hundreds (ideally thousands) of PVS patients. This is not a condition where you want to be someone’s first case.
Framework over randomness. The provider should articulate a clear treatment framework based on root cause mechanisms, not just “let’s try this and see.”
Realistic expectations. Be wary of promises of quick cures. Trust providers who are honest about timelines and success rates.
Strategic approach to testing. Good providers don’t reflexively order $5,000 in labs before starting treatment.
Individualization. While the framework should be consistent, application should be personalized to your specific presentation.
What to Expect from Your First Appointment
A good initial evaluation should include:
- Comprehensive symptom history
- Timeline of symptom onset and progression
- Review of treatments already tried
- Assessment of which root mechanisms are most dominant in your case
- Discussion of treatment framework and what to expect
- Clear explanation of therapies, mechanisms, rationale, etc…
- Treatment plan you actually understand
How Leading Edge Clinic Can Help
We’ve specialized in treating post-viral and post-vaccine conditions since 2022. We’ve treated over 3,500 patients with Long COVID, Post-Vaccine Syndrome, and related conditions.
Our approach:
- Comprehensive treatment targeting all seven root causes
- Strategic, individualized protocols
- Minimal unnecessary testing
- Nationwide telehealth (available in all 50 states)
- Monthly monitoring and adjustment
- Honest expectations and proven outcomes
What makes us different:
- We’ve seen what works and what doesn’t across thousands of patients
- We understand the biological mechanisms deeply (spike persistence, immune dysregulation, CDR, redox, microclots, ANS, senescence)
- We don’t use cookie-cutter protocols
- We focus resources on treatment, not excessive testing
- We’re honest about timelines and realistic about outcomes
Ready to Start Your Recovery?
If you’re ready to move beyond failed treatments and address the root causes of your Post-Vaccine Syndrome, we’re here to help.
Register as a new patient: https://drpierrekorypatientportal.md-hq.com/registration
Questions before scheduling? Contact us at info@drpierrekory.com or (608) 400-0141.
What to bring to your first appointment:
- List of current symptoms and severity
- Previous treatments tried and results
- Current medications and supplements
- Recent lab work if available (not required)
- Your questions and concerns
A Final Word
We know how frustrating and isolating Post-Vaccine Syndrome can be. You’ve probably been dismissed by doctors, doubted by friends and family, left to figure this out on your own.
You’re not imagining your symptoms. You’re not “just anxious.” You’re not “getting old.” And you’re not doomed to feel this way forever.
Post-Vaccine Syndrome is real. It has identifiable biological dysfunctions. And it’s treatable.
Yes, recovery takes time. It requires a strategic approach. And yeah, you need the right medical guidance.
But with proper treatment addressing all seven root causes? Most patients achieve significant recovery. You can be one of them.
You deserve to feel like yourself again. You deserve to be believed. And you deserve proper care.
We’re here when you’re ready.
Disclaimer: This article is for informational purposes only and doesn’t constitute medical advice. Post-Vaccine Syndrome treatment should only be undertaken with qualified medical supervision. Don’t attempt to self-treat based on information in this article.
About Leading Edge Clinic
We specialize in treating post-viral and post-vaccine conditions—Long COVID, Post-Vaccine Syndrome, MCAS, and related disorders. Since 2022, we’ve treated over 3,500 patients nationwide via telehealth. Our approach is based on understanding and addressing the root biological dysfunctions that drive these conditions.
Learn more: drpierrekory.com