Notes to the reader: if the Substack is truncated in your email, click on “View entire message” and you should be able to view the entire post in your email app. Comments and the final plan of care are restricted to paid subscribers for this post. Some of the links are not active, because this post is so long.
35 year old male
Has a benign medical history, eats very healthy, and prior to injury, exercised a lot. Eventually determined that he had overtrained and over-dieted which led to a low testosterone issue. Was a field scientist, and went back to school for a health profession. Most of 2022, was at his apartment for 18 hours studying and sleeping, or going to class.
Patient initially presented 7/11/23 for telemedicine consultation re: symptoms following acute COVID-19 infection and COVID shots. Referred by his functional medicine mold specialist.
– Health status: stable chronic. Hx CIRS, hypogonadism, exogenous testosterone S/p Muscle biopsy and dehiscence semicircular canal
– COVID-19 vaccination status : x2 mRNA Moderna
BATCH ADRs DEATHS DISABILITIES LIFE THREATENING ILLNESSES
013L20A 3119 62 39 26
023M20A 1616 23 17 31
-7/5/23 spike antibody IgG 10,090 U/mL
– Previous COVID-19 infection by testing or presumptive by symptoms, December 25, 2022.
– Onset of symptoms December 2022 and constellation of symptoms including fatigue, brain fog, memory problems, shortness of breath, dizziness when standing, fast or pounding heart rate, loss of taste or smell, anxiety and depression, symptoms worsening after activity. Also reports burning muscle pain, fiberglass skin sensations, stabbing upper and lower back pain, muscle twitches and “blood pumping in legs” sensation
– Clinical trajectory: worsening.
April 2022 was diagnosed with hypogonadism. Had fatigue, wasn’t gaining muscle while working out, libido was low, was cold all the time. Total testosterone below 50 ng/dL, and was started on exogenous testosterone therapy with internist. Had researched therapy, shifted to a hormone specialist with an aromatase inhibitor (AI) and higher dose of testosterone. June 2022 had a back injury with weightlifting. Did physcial therapy. Symptoms started to pile on. Thought the AI was the issue. Came off both testosterone and AI after a couple of months. Between insurance and appointment scheduling delays it took months for tx. Scheduled twice for a muscle biopsy. Looking at Multiple Sclerosis and autoimmune illness. Did labs, nerve conduction study, muscle biopsy, brain and then spinal MRIs. Went to Neurologist, who said this was post-viral illness, and given medication (uncertain what meds).
Found his way to a functional medicine physician who focuses on CIRS and mold toxicity, first visit January 2023. Had Genie testing: https://www.survivingmold.com/resources-for-patients/treatment/genie-genomic-expression-inflammation-explained-now-available. Was living in an apartment which had high levels of mold. Moved out, started to get better with treatment, and then got much worse.
Activity makes him worse. He has to be careful about walking more than ten minutes at a time. He can’t lift anything without it causing a flare of his symptoms. His muscles burn when he uses them. He’ll have a “fiberglass” symptoms affecting his skin systemically. Was wearing shorts, no socks. Typically feels cold. He has stabbing back pain all the time. Has sporadic muscle twitching. He couldn’t think at all, or remember what he expect to be able to remember. “My legs are always vascular, especially my left one all the time.” He feels a “blood pumping sensation”, used to happen all the time, went away, and then came back.
He had drowsiness during Summer 2022, and couldn’t work even part-time. He would be studying during summer courses, and would get up early in the morning to get a couple of hours of studying in; this lasted a few months, but recently came back some. He was trying to start some classes in August 2023, and was struggling with self-worth, because he “isn’t doing anything.”
***He has had some anxiety, depression and suicidal thoughts, which is completely new. When pain went away, those feelings would go away. More recently, even without the pain, he would have those feelings and thoughts. On a good day this typically goes away.
June 30th, 2023 he started IVM. Within days, the anxiety and depression disappeared.
Physical symptoms seemed to be getting better. Started ATP360 6/23 and hadn’t noticed any difference. One of the few things which improved was his libido.
IMPRESSION: Constellation of multi-system symptoms NOT temporally associated with vaccination for COVID-19, BUT temporally associated with episode of acute COVID and consistent with vaccine injury. Patient received two mRNA shots from bad batches. Symptoms reflect mitochondrial damage, endothelial inflammation, anti antibody response, and micro clotting, with a no signal of mast cell activation (initial impression). Provocation and exacerbation of injury facilitated by testosterone use (enables spike entry into cells via TMPRSS2 pathway).
Discussion: You are taking Colsevelam/Welchol (as a binder Rx by your mold specialist). As we discussed, cholesterol is both the constitutional basis of building hormones in your body, and is utilized in your mitochondria to make Progenolone, which is your own endogenous steroid, that helps lower systemic inflammation. Your last testing of this level is in the 50s ng/dL, which is suboptimal. My suggestion is to stop this medication and permit at least four days to evaluate for change in your symptom burden. In the short term your blood lipids will increase. Within six months, they will be better than previously. Four days after discontinuation of Colsevalam, I would suggest initiating Nattokinase per my directions, which will modulate your blood lipids, and more importantly, help heal the lining of your blood vessels, while breaking down microclots and neutralizing spike. Because Nattokinase heals the lining of blood vessels, your blood pressure will improve. You should check your blood pressure daily, and expect that you will need to stop taking your Losartaan for BP control. As your systolic BP approaches 120 mm/hg or less, it would be best to cut back or eliminate this medication.
The Desmopressin which you are taking, for reasons which are unclear to me (mold specialist later explained conern for decreased cardiac preload secondary to disregulation of anti diuretic hormone or ADH), is most likely harming you. Please see the attached study re: the development of autoantibodies following acute COVID which attack ADAMTS13, the enzyme which manages clotting in our body. When ADAMST13 is driven down, it drives up vonWillebrand factor levels, and both changes increase your body’s tendency towards clotting. It is very likely that you already have significant microclotting at baseline due to vaccination and spikopathy. If you use the free software Epocrates to understand the pharmacology of Desmopressin, you will learn that the mechanism of action leads to increased plasma Factor VIII and von Willebrand factor levels. This increases the risk of clotting in the context of vaccine injury and autoimmune dysregulation.
DRAFT SCHEDULE: Spacing changes is important in order to assess for benefit, neutrality and side effects.
Day 0 Pacing is the single most important intervention in surveys of vaccine injured by REACT-19. See the presentation about this by Dr Joel Wallskog of REACT-19 from the FLCCC Conference in May 2023.
Day 0 DC Desmopressin
Day 0 Intermittent fasting. Long-term goal should be at least one 72 hour fast per month.
Day 0 Continue with IVM daily. Target at dose of 0.4mg/kg, divided into two doses daily with food and fat.
Day 4 DC Colsevalam
Day 8 Nattokinase 2000fu (100mg) orally on an empty stomach. Take this daily for two days, and then increase to 4,000fu daily. As tolerated, advance by adding an additional 2,000fu later in the day at least two hours after a meal and at least thirty minutes before the next meal.
Day 12 Take NAC Augmentata (NAC-A) 200mg orally once daily for a week to determine your tolerance. You may feel some minor return of previous spike related symptoms as your body begins to break down the fragments from spike denatured by the NAC-A. Then take twice daily for up to three months, or until resolution of symptoms, and then daily indefinitely. You can take it with food, but I have found that best effect is to take on an empty stomach, or at least 15 minutes before eating. Drink plenty of water, i.e. at least 16 ounces with each dose, when taking NAC-A.
Day 16 LDN 0.5mg/drop, starting with one drop under tongue at night for one week, advancing as tolerated up to 4.5mg.
Reassess after 2-3 weeks.
***If iliac venous compression (IVC) continues untreated, it is possible (I have seen this in at least four patients) for neuropsychiatric symptoms to emerge. Post acute sequelae of COVID (PASC) and vaccine injured patients are often misdiagnosed as having psychiatric issues and treated with a raft of antidepressants, antianxiety and antipsychotic medications which don’t address the underlying and undetected pathophysiology. My working understanding of the pathophysiology of IVC is as follows: IVC or May Thurner Syndrome (MTS) exists in 30-40% of the population as detected on autopsy, but many people pre-pandemic were asymptomatic during their lifetime. The origin of this condition is an anatomical vulnerability. The left kidney sits higher than the right in most people, and as a result, the right iliac artery crosses the left iliac vein in a manner which increases compression. The spike protein from the COVID shots enters the bloodstream and provokes both direct and indirect injury to the endothelium (cells lining the blood vessels). I have seen IVC in an unvaccinated individual, so that I think high spike burdens from shedding can contribute to this condition. Spike also provokes microclotting and causes injury to the collagen which provides structure to compressible veins.
The perfect storm which appears to provoke IVC in PASC and vaccine injury patients is a combination of anatomical vulnerability, vascular injury, widespread coagulopathy, and resulting pelvic hypertension with venous stenosis, reflux and collateral flow that decreases the preload to the right atrium (results in POTS). The pooling blood in the pelvis provokes ongoing systemic inflammation, irritating and impacting surrounding organs, such that we can see in the labs impaired renal and liver function, and irritation to the bladder causing cystitis, and the gut, causing dysbiosis. MCAS flares in such patients.
Historically, IVC and MTS was associated with young woman of child-bearing age, and symptoms including left leg pain and swelling, pelvic pain, and lower back pain. In the more than sixty patients I have worked up for IVC, there have been men and women of all ages, less than half of whom have any left leg symptoms or even pelvic pain. Most of them have an athletic history. Many have a history of trauma or surgeries or both affecting the abdomen and pelvis. Men often have history of left testicular varicocele. Woman may have had multiple pregnancies. Development of urinary urgency, frequency and nighttime voiding is common, as well as dysbiosis (constipation, diarrhea, bloating, heartburn, abdominal pain), new hemorrhoids, painful intercourse for women, POTS and MCAS. A minority of patients have lower extremity edema and new varicosities. Dyspnea, chest pain and headaches are not uncommon. Increased anxiety, depression and insomnia or poor sleep patterns are common. Coagulopathy, with consistently elevated microclotting scores is uniform, and it is not uncommon that elevated D-dimers are found. Patients often feel worse in the morning and get progressively better during the day.
7/28/23 Recently has experienced an increase in his symptoms. He started NAC-A about four days ago and is correlating the increase in pain for when that started. I explained to him the process of denaturing spike and how we can see patients have an increase of symptoms during the initial start of taking NAC-A. He is only taking 1 cap daily. I suggested that he go down to 1 cap every other day, but he wishes to continue taking it daily knowing his symptoms may improve after a week or so. He clarified that he is off of the Atorvastatin as well as the Colesevelam, but is still taking the Desmopressin to finish off the bottle.
7/30/23 I was able to speak with his mold doctor via phone for an hour. He utilizes the Shoemaker Protocol in treating CIRS patients. Notable excerpts from our conversation reflecting his clinical thought process include:
With pulmonary hypertension, patients will have elevated right-sided pressures, and so have less blood return to right side of heart. Can only increase stroke volume or heart rate. With POTS, the first thing he does is look at specific gravity and it is typically 1.10, indicating intravascular volume depletion. With Desmopressin, increase ADH, which improves intravascular volume and eliminates passing out. Try to reset hypothalamic output of ADH. Proopiomelanocortin (sic) pathway is disrupted.
***This is a very important part of the history, as the mold doctor was on the right track with concern for decreased preload, the volume of blood returning to the right side of the heart and this leading to POTS symptoms, but the pathologic cause was actually iliac venous compression and coagulopathy, not changes in ADH.
The physician thinks that the patient got much worse due to exposure to a water-damaged building. He had gone to visit his mother, and staff had documented issues with her home. Was wearing long-sleeves and shirt in June 2023, first time able to do this in a while. Skin culture showed Propionibacterium acnes (gram positive)…. was >200,000, and should less than 10,000.
***Another important point, because mold practitioners are inclined to blame mold as the primary souce of the patients troubles, when it is more likely that the spikopathy from COVID infection and vaccine injury has destablized mast cells, provoking MCAS and lowering the patient’s tolerance of pre-existing environmental mold.
Historically there is a relation between CIRS and increased vonWillebrand, and thus increased clotting. He hasn’t noted previous microclotitng with CIRS, but hasn’t had a manner of testing it.
Discussion of and agreement re: use of micro current therapy going forward.
08/15/2023 Telemedicine visit
Not very much is going well.
Just finished abx, going to Peridontist, who will be removing an implanted left upper tooth.
His pain wants him to say that everything is worse. He’s trying to be realistic about what is worse. He struggles to go to the mailbox. Got up yesterday to make breakfast for his girlfriend. Getting up and walking to the kitchen feels like a big workout. Back in January 2023 he could still move himself into his kitchen.
Wakes up with burning and stabbing pain, hyperalgesia. Clothes hurt. Has lost half of his hair, starting about a year ago. He can feel every hair which falls off his head, and it is worse.
He is experiencing a lot of stress, and it has gotten into his head. Got rid of his bed and couch, and had his apartment cleaned professionally. Got his workout bench out of storage, and is looking at it, wondering if it has mold.
“I’m tired of fighting, and don’t want to be here. I’m telling everybody so that doesn’t happen. My life is trying to be a good boyfriend, because I found the woman of my dreams. I’m doing one college class, and it’s hard. In the past, I could do that in my sleep, but now I’m tired, in pain, and struggling.” Would prefer to physiologically feel better before reaching out for psychological therapy and cost is a concern.
Cold all the time, but burning and stinging is mostly in legs, and going everywhere, including now in his face. His skin is very wrinkly, which started a while back. Unless the mold and bacteria are the issue. He overthinks eating, his relationship, his finances.
His girlfriend ran a race this last weekend. “Everyone’s life is going elsewhere.”
Mold doctor indicated to him that we were on the same page, but wanted him to keep taking the Cholseval and VIP (vasoactive intestinal peptide, nasally administered). The VIP is used in CIRS “to attack several biomarkers.” It’s the only thing which feels like it has for sure helped him.
He ventured a theory: references Dr Jordan Vaughn’s statement that he has a large segment of patients who can identify the day that they were injured. The only thing which changed before injury was starting to take testosterone. Then, he was deadlifting and had a lower back injury while deadlifting. The day his skin sensation/pain started, was the week he had a muscle biopsy, cold-turkey quit nicotine, which he understands to open the floodgates to spike in the brain. He can wake up and his left leg is “super vascular.” He would look at it every day, and it would upset him.
***Another key point in his history, as many IVC patients can pinpoint the day and time when their life dramatically changed for the worse.
7/11/23 Telemedicine visit
“My legs are always vascular, especially my left one all the time.” He feels a blood pumping sensation, used to happen all the time, went away, and then came back.
No Hx of left testicluar concerns. Has Hx of hydrocele on his right. Mornings used to be manageable, and things would go downhill over the day. For fourteen months, he has always slept very hard. The last several weeks have been the hardest of his life. He wakes up with hope and fight, pushes through his day, and by the end of the day, he doesn’t want to talk to anyone. Mornings now suck, because he started in pain. Hasn’t noticed any edema in his legs.
He is on day three of the Arc device. He can perceive the micro currents.
IMPRESSION: Severe post-exertional malaise secondary to mitochondrial dysregulation and hypoxia from extensive microclotting. Left iliac venous compression: specific time of onset, following possible pelvic injury, severe lower back pain, left LE vascular prominence.
PLAN:
-Please complete the vascular study ordered to initiate workup for left iliac venous compression. This is the first step towards completing an MR venogram which would provide the definitive diagnosis and is needed by a vascular surgeon.
***I ordered vascular studies on the first tweny or so patients until I realized how useless they were in diagnosis.
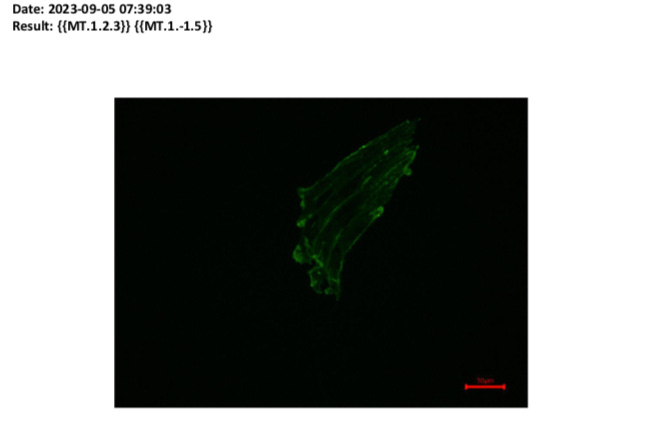
-Please complete blue top testing with Dr Vaughn to evaluate/stage microclotting.
-Please consider completing the labs which were ordered during our first visit.
Day 0 Initiate Plavix 75mg orally daily.
Day 4 Initiate Aspirin 325mg orally twice daily with food.
Day 8 Initiate Eliquis 5mg orally twice daily
8/23/23
Day 8 of the anticoagulationt reatment plan.
Some increased numbness in right arm. “My muscle burning (predominantly legs), back pain, and energy have without a doubt noticeably improved. My fiberglass skin pain has improved maybe slightly. “
9/6/23
A couple of bruises here and there but no negative side effects of anticoagulation other than the numbing in right arm. Can walk more and exert himself a little more with less pain and less repercussions. His three main symptoms are stabbing back pain, burning muscle pain, and hyperalgesia that he refers to as fiberglass pain where it hurts just to wear clothes. All are exacerbated by activity (walking, lifting, exercising). Two of the three were improving last week, back pain was not getting better.
9/18/23
Microclot results are back: stage/grade 4 of 4 amyloid fibrin microclot formation, significant and widespread.
09/28/2023
Having some improvement. Waking up each day with a better attitude, because he has some answers re: what is causing his symptoms, i.e. microclotting.
Week two of triple therapy he was able to walk across campus. He overdid it during that second week; went on a long walk with his girlfriend, walked across campus twice, and helped new neighbors move into their home. His brother’s truck needed a new battery. It is elevated, and for 1 1/2 hours he was picking up the battery and moving it around. His upper back was excruciating for the following two weeks. He also had an acute episode of presumed viral illness.
He also had his dental implant removed, and started feeling better last week.
The fiberglass sensation affecting his skin is up and down. If he does too much, everything will get worse.
Before MRI of his spine in 12/22, he could feel the blood pumping through his legs and the twitching. Discussion of whether or not to repeat MRI, or wait until his previous MRI has a second read by Interventional Radiology specialist Dr Brooke Spencer in Denver, CO.
Discussion of Aspirin 81mg daily vs 325mg twice daily. Mold doctor has concerns re: large doses harming him.
***Worth noting that higher doses of Aspirin could have helped mitigate his MCAS symptoms, but may have led to earlier incident of rectal bleeding, which occurred three months later when the patient increased Aspirin dosing to 81mg BID and was straining to have bowel movements. Ongoing use of the Arc Microtech has minimized concerns re: bleeding and bruising in our patients on anticoagulation therapy.
IMPRESSION: Stage/grade 4 of 4 fibrin amyloid microclotting, experiencing clinical benefit with triple anticoagulation therapy. Suffering increased symptom burden following overexertion, recent acute viral illness, dental surgery, and ongoing shedding exposure from increased social contacts with school and medical/dental office visits. Concern for iliac venous compression (IVC). We identified a previous non-contrast MRI thoracic/lumbar spine, and with some small chance it could provide clinically useful information. If not, we can order an MR Venogram.
PLAN:
-Send CD of MRI Lumbar and Thoracic spine from 12/22 to Dr Spencer’s office Colorado for an overread (medical term for second opinion radiology review)
-Rotate sites with Arc device. Order more self-adhesive pads from the UK.
-Order for Nattokinase from Allergy Research Group sent to FullScript. This formulation may have a special advantage for you, because it has low or no histamine and may be less provocative to your system with mast cell instability, and histamine release from breakdown of platelets.
-Feel free to take (mold doctor’s) direction to use only Aspirin 81mg daily instead of Aspirin 325mg twice daily, if upon reflection of our discussion you have lingering concerns.
-Sip Baobab 1 Tbsp in 16oz water over at least eight hours daily.
10/12/2023 RN followup call:
He is doing okay, having some days of feeling good mentally and physically. Not having the fiberglass pain when putting on clothes and being able to move around more. He will then have days that follow that he doesn’t feel well, low energy, clothes cause pain and can’t tolerate moving around much. He continues on the anticoagulant therapy and is tolerating it well, without concerns of bruising and bleeding. He is scheduled to have telemedicine consult with Dr. Spencer’s office on 11/1/23. They are talking about doing the MR Venogram and he is wanting to get that completed. It sounds like they will order it for him to complete locally.
10/27/2023 RN followup call:
He will have days that are considered good days. His clothes will feel okay and not cause pain, he is able to walk longer distance and mentally has more energy and clarity. Other days that are not so good, he is in a lot of pain and exhausted. During these days he feels mentally down and questions wanting to live. This was more frequent in the past. He states he is very vocal about this to his family and does not have a plan.
11/17/2023 Telemedicine visit
Repeat MR Venogram didn’t occur. The night before the study was supposed to happened the imaging center called and said that they don’t do MR Venograms. Now he is communicating with staff at Dr Spencer’s office, and they advocating for him. They have patients on the East Coast who they have sent to a local academic medical center which is about an hour away from him.
***Arranging for local MR Venogram is an uphill and time-consuming battle for our staff and the patient, and we have had to start charging for the hours spent on it. Insurance doesn’t want to pay for it. At least a 3T magnet MRI is needed. Technicians, schedulers, radiology nurses and physicians are often unhelpful and do not distinguish between the venous study we want and the study they perform. Local radiologists almost uniformly do not correctly read the MR Venogram and do not identify venous compression, but it can be identified by Dr Spencer and her expert Interventional Radiology (IR) team. We have to arrange for a CD copy of the study to be sent to Colorado for a second opinion. Vascular studies including locally performed ultrasounds are almost completely useless in identifying IVC. I have spoken with more than twenty (!) vascular surgeons and IR physicians across the United States, and only three have been capable of having a reasonable conversation. The rest have been condescending in their “expert” lectures to me about May Thurner Syndrome (MTS) or IVC, and how a patient who doesn’t fit into the box they are familiar with, could not possibly have the condition, let alone could it be caused by spike protein, let alone have it lead to neuropsychiatric symptoms.
“I want it to be something, but I’m not doing any better.” The short walk to class is now fine with the triple anticoagulation. Walking more than that brings negative repercussions. He has been hopeful between now and then. If he overexerts a little bit, the next week he has a lot of pain.
He ran into something a few weeks back and had bruising. The initial numbness in his arm and increased bruising with initiation of anticoagulation has resolved.
Discussion of Flavay and Sulodexide, and potential benefit for collagen repair. A few months into his health issues is when his skin started looking old and then exfoliating. He is also losing muscle mass. Recently, inside his right ear, the skin is exfoliating. Anytime he overdoes it, his hair will start to be less soft and fall out faster.
Two weeks ago he had a very bad week. He thinks it’s because he overexerted the week before, and then started struggling with dark thoughts, and his hair started falling out more.
He is cold on a regular basis, despite wearing extra clothes. Compression underwear with polyester and cotton helps the pain from wearing clothes. If he walks too much, the fiberglass pain returns. It’s 73F in his apartment, and he has a heater on, with compression underwear.
He stopped the Arc, because it was leaving marks on his arm. Discussion of how to rotate sites, avoid constriction, and use it on his ankle with medical tape.
If the MR Venogram comes back clear and it isn’t that, then what will we do next?
Traditional Chinese medicine (TCM) drops, Sulodexide, Flavay.
IMPRESSION: Plateau in clinical progress. Ongoing exposure to shedding from class attendance. Delicate balance with post exertional malaise, extreme temperature dysregulation, hypersensitivity of skin, hair loss, decreased skin turgor, muscle atrophy. Baseline elevated spike ab dilution and stage/grade 4 of 4 amyloid fibrin microclotting. Concern for iliac venous compression.
*** Improvement in clinical symptom burden with initiation of anticoagulation, followed by plateau and/or regression is a common feature for patients with IVC.
PLAN:
-Use a styptic pencil from a local drug store to stop facial bleeding when you cut yourself.
-TCM eye drops and nasal spray to protect against spike shedding.
-Over-the-counter therapy to inhibit platelet adhesion to blood vessel walls, which is an over-the-counter equivalent of Plavix: Flavay 100mg (1 cap) twice daily. Advance to 200mg (2 caps) twice daily as tolerated. Flavay is available online at: https://www.healthysource.com/flavay.html
-Pentoxifylline (PTX ER), 400mg three times daily. It is third-line therapy in patients with severe microcirculatory disturbances. PTX is a non-selective phosphodiesterase drug that has anti-inflammatory and antioxidant effects. It improves RBC deformability and reduces blood viscosity, so can mitigate the hyper-viscosity and RBC hyper aggregation, which is linked with the development of coagulopathy in the vaccine injured. It is also an PAI-1 inhibitor, which enables the body to break down the microclots more easily. Cost isn’t prohibitive, $15 for 60 tabs with Good Rx coupon.
-Restart the Arc in two weeks on program 3, then a week on program 4, then rotate a week each on program 1, 2, 3 and 4.
-See attached reports re: Sulodexide https://pubmed.ncbi.nlm.nih.gov/36769668/ and https://pubmed.ncbi.nlm.nih.gov/35647070/.
12/4 Telemedicine visit
Patient reports 12/1/23 appt with NP in Dr Spencer’s practice, and review of lumbar spine MRI from 2022. Overread revealed severe left iliac vein compression. His dad is flying him to CO and has appt 12/11/23 for MR Venogram. Dr Spencer’s office is going to update this week but trying to arrange for stent placement while he is out there.
Patient reports NOT feeling any better at all. Admits now that he has had blood in stool on/off since starting blood thinners but didn’t think much concern of this and therefore did not relay this information until now. Reports since changing to Flavay he has now had significant amount of bright red blood daily in stool, splatter in toilet and when wiping. Denies SOB, dizziness, lightheadedness, nausea or vomiting. Is currently on 81mg Aspirin, Flavay 2 capsules BID, Pentoxifylline TID but has discontinued Plavix when he started Flavay. Using ARC on program 4. Has not required styptic pen as trying to shave more frequently and thus noticed less issues with knicks/bleeding.
Advised we will follow closely regarding the concern of bleeding above and the importance of informing us of this type of issue. Verbalizes understanding. Later acknowedged to nursing that he had bumped up Aspirin to 81mg twice daily.
Plan to get a CBC, CMP and guaiac of stool to assess for blood loss. Back off Aspirin to twice weekly. Rotate Arc each week through programs 1, 2, 3, 4. Ship TCM eye wash and nasal spray to him before his flight, as the shedding in the airport and on the plan could be very harmful for him. He can/should also order Enovid nasal spray from Israel.
-Utilize ENOVID Sanotize nasal spray from Israel up to six squirts total daily during your travels. You can use this spray before departing for the airport. This can be ordered online at this address: https://buyenov.com
12/4/23 Telemedicine consult read of 12/14/22: MRI Lumbar performed at OPI.
There is severe left MIV compression with a moderate length stenosis. The internal iliac on the left is dilated suspicious for presacral plexus collaterals. There is no signfiacnt disc disease. Venography and intravacular US with left renal venogram can be considered with possible iliac vein stenting.
12/5/23 RN follow up call
No further rectal bleeding since drop of Aspirin to 81mg twice weekly. CBC, CMP normal. Stool test negative for blood. Likely blood was from a hemorrhoid secondary to IVC and straining to have BM with constipation.
12/7/23 Labs, note from provider
Thanks for getting these labs done. Overall, I find good trends in these values. I don’t think the low WBC or RDW is clinically significant. Decrease in MCHS tells me that you’re freeing up movement in your capillaries for the RBCs to deliver O2 and remove C02, so that your body isn’t loading as much hemoglobin on the RBCs. BUN and BUN/Creatinine ratio improved a notch, while Creatinine increased slightly, a good sign for renal function. Platelets improved, meaning less are getting chewed up in microclots, and your bone marrow is functioning well. Albumin (protein in blood) has normalized. Liver enzymes have improved, and your stool was negative for blood.
WBC 2.9, RDW 11.3, MCHC from 34.3 to 33.5, Plts from 240 to 255, Albumin normalized, BUN 22 to 22 mg/dL, AST 32 to 19, ALT 43 to 17.
12/19/23 Procedure note
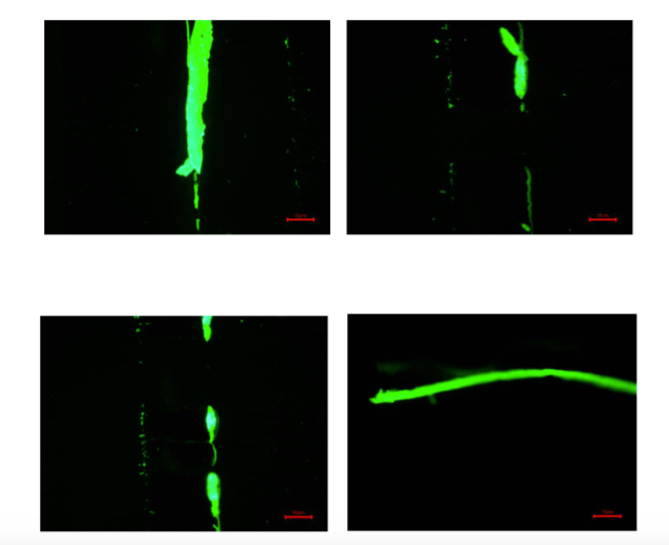
The Inferior Vena Cava measures 431.8 mm square in cross- sectional area. The left Common Iliac Vein measures 284. 9 mm square in cross-sectional area where normal with a 56.% stenosis in the tightest area. The left External Iliac Vein measures 165.9 mm square in cross-sectional area. Additional measurements were performed including diameter of the narrowest portion of the common iliac vein which was 4-5 mm compared with approximately 18 mm diameter of the normal common iliac vein which would represent a 73% stenosis in diameter. Although his degree of compression was somewhat equivocal, his venogram does demonstrate severe reflux, therefore the decision was made to proceed with stenting.
12/22/23 No further rectal bleeding and in response to report of constipation s/p stent placement, OxyPowder ozonated Mg recommended to help with BM regulation.
01/08/2024 After completed the stent placement, reports no real significant changes in symptoms. Fiberglass sensation is still present, maybe slightly improved. Energy is still low.
01/19/2024 Telemedicine visit
“I’ve had huge improvement.” He was sick, tired and the three weeks after surgery were not fun. He noticed after surgery that he had a huge release in the fiberglass pain which lasted for a while, but all the other pain was terrible. It was hard for that to be appreciated amidst the other discomfort. He was however wearing more clothes. Three weeks post-surgery his post-op back pain was terrible. In the last two weeks he feels like he has improved every day. His fiberglass pain is better, holding steady. He is wearing more clothes, touching more things. Post-op and chronic back pain form the last 1 1/2 years is better. Burning muscle pain is better. Activity level has doubled, but mental capacity feels like it has gone through the roof. “Right now I’m handling all kinds of stuff. I got a part-time job teaching at the university, and am taking two instead of one class. My truck needs repair, but I’m looking into fixing that myself, and I’m taking on more things.” He caught himself going on walks just to go on walks, after being terrified of walking across campus. Now with two classes, that means walking to two different locations.
Previously it would take him a week of doing nothing to recover if he walked to two different locations. Now he is walking more, intentionally, with a big backpack with a lot of weight. The only people who knew before yesterday how well he was doing were his mom, girlfriend and a close friend. “I feel scared to say it, but starting yesterday, I’m just going to say that I’m doing great and keep moving in that direction.” There have been a lot of family and friends praying for him.
No symptom has completely resolved. He is not yet at his normal mental capacity, to take on a part-time job and full course load. He still has some back pain and fiberglass pain.
He went on a fifty minute walk before our meeting and feels fine. He can still feel increased blood pumping in his legs, which has been present from the very beginning. “Something is going on there.”
Money has become a big issue. He wants to discuss how to trim medicines from the list.
He came off LDN for surgery, and hasn’t restarted it. He has a good supply of NAC-A, Nattokinase, Eliquis. He had a big reserve of IVM from India, but is about to run out in two weeks. He needs Flavay, about to run out. He did the Arc and Baobab consistently, but the Arc is a hassle. He did the Arc for two weeks after surgery. The Arc hurts him during a three hour cycle. He only ever used the thick carbon pads, because it only came with two of the self-adhesive pads. Using TCM one drop of eye drop in each eye, and one spray in each nose. The eye drops stained his contacts. He hasn’t noticed any negative effect, but stopped putting them in when he wears his contacts.
IMPRESSION: Significant clinical improvement following iliac venous stent placement with increased cognitive function, exercise capacity, decreased fiberglass pain. Decreased chronic back pain. Intense concern re: financial constraints and need to trim therapeutics in order to maintain benefit, but stay within budget.
PLAN:
-Invite to support group Thursday 8-10pm.
-Shift to normal Nattokinase from NK-SD for cost concerns.
-DC Pentoxifylline, due to lack of demonstrable benefit.
-DC fish oil for cost.
-Pause Flavay for cost.
-Change Aspirin to 81mg daily
-Continue IVM 12mg daily (reduced dose for cost)
-Restart LDN to stabilize mast cells, tighten cellular junctions of gut for leaky gut
-Use Arc for three hours a day rotate each week through program 1, 2 and 3. You can use saliva instead of gel to make contact with the carbon pads.
02/06/2024 RN followup call
The Monday after our last visit, he experienced a return in all of his symptoms. The day of his visit he had made the adjustments of stopping some meds and supplements and decreasing others. He was wondering if he can go down to 1 cap daily of NAC-A augmentata instead of 2 BID to save on cost. He has been taking 1 cap daily recently and hasn’t noticed a difference in symptoms. ***He made all of these adjustments right before he experienced the crash***, but it has been 2 weeks now and he is starting to feel better. He believes he overdid it with how much he has pushed himself the weeks prior. He is not back to feeling as good as he did before, but it is improving. He is tolerating walking to campus and his pain is decreasing. We discussed nutrition habits and he feels fasting puts a stress on his body. I encouraged him to just focus on waiting to eat 1-2 hours after waking up and avoid eating at least 3 hours before going to bed, but then during the day eat low-inflammatory foods. He discussed having the habit of eating right before falling asleep after a long day of working and studying. I encouraged him to schedule breaks throughout the day from studying and dedicate an hour for dinner to enjoy a sit down meal with his girlfriend. This will help him metabolize his food before sleeping, but also manage his stress during the day. He agreed and plans on implementing this. He has decreased the amount of physical activity he is doing to not over do it and is tolerating it well.
02/16/2024 Telemedicine visit
Two weeks of severe downturn with physical and mental pain after two weeks of tremendous physical relief at third week s/p stent placement. His mindset changed completely from being rock bottom to thinking about marriage, graduate school in a health profession, and moving forward in the near future.
He had a busy week with exams and work. School and work keep him busy 24/7. He and his girlfriend decided to pick up a babysitting job for four days in the middle of his exams. During that time he started to feel better, after going into that feeling pretty crumby. He got very little sleep, then got sick Thursday a week ago. He couldn’t sleep and was getting behind on school and work. ***In the middle of being sick, despite not sleeping, he didn’t decompensate.*** Normally he needs at least nine hours of sleep.
“I want to get better, heal, and go back to my normal life.”
A thought a few days ago was that he felt better the next day after starting anticoagulation medication. With Aspirin, he went from not wanting to move to being happy to go down the steps. This raised questions in his mind about dependence upon medications. “I want to feel better because I’m truly healing, not because of some pill.”
All of his pain is decreased. Last night slept eight hours. This week he walked around campus with his backpack for the purpose of walking. He added in the extra paces because he was feeling good. Going non-stop from 6:30am to 10:30pm. Back pain made it hard to drive to school, but he can now drive with less pain.
He reflects that it’s easier for him to make decisions which are on behalf of others than himself. In the shape he is in right now, he can’t be a father or go to school, and if someone tells him that he can’t do those things, it is hurtful. His teaching commitment ends beginning of May, and he has been asked to teach another class from August to the end of November 2024.
He has certain clothes which he has set aside, because it isn’t tolerable to wear them due to the fiberglass pain. Sometimes he will try them on to test them. Cotton has been his favorite fabric, and today for instance he is able to wear a cotton sweatshirt, which doesn’t feel great, but can bear wearing.
IMPRESSION: ~ Two months s/p stent placement for iliac venous compression. Global improvement in the last two weeks with decreased lower back pain, improved cognitive function and stamina. Fiberglass sensations/pain remain at a decreased level, which may yield to treatments focused on neurological improvement.
PLAN:
-Live02
-Titrate Aspirin for benefit, e.g. up to 81mg twice daily with Arc to limit bruising and bleeding.
LITHIUM MICRO-DOSING
-Lithium is a trace mineral which may help prevent and treat neurological conditions secondary to spikopathy. Dosing is ~130mg orally daily. That dosing is many times below any level of potential toxicity. It can be purchased online for about $15 for six months worth from this source.
https://horbaach.com/products/lithium-orotate-130mg-180-capsules
Below is a link to the Substack by Dr Michale Nehls on the topic of Lithium.
L-ARGININE
-Trial L-Arginine 1500mg together with Vitamin C 500mg orally twice daily for four weeks to support energy and endothelial function. See this study: “https://pubmed.ncbi.nlm.nih.gov/36501014/”.
03/04/2024 RN followup call
He was justting getting over his recent acute infection and has now come down with another acute infection. He had never started the NTZ and HCQ due to receiving meds after inection was resolving. He had ordered them anyway to have on hand. Last week he would feel fine during the week, but then at night would cough and didn’t sleep much. Saturday he felt tired, but thought it was from overdoing. Sunday he woke up with body aches, fever of 99F, sinus congestion and continues to cough. He started NTZ and HCQ right away. He is also going to pick up the Azelastine spray for nasal congestion. He states his cough is productive and coughing up green sputum. Last week, despite being sleep deprived he was able to function better than he normally would. Post exertion malaise has improved and fiberglass pain has slightly improved.
03/11/2024 Telemedicine visit
“I’m doing great.” “It’s been a rough month, but I’ve been very happy.”
Five weeks of getting sick three times was challenging. The problems he was being treated for were getting better during that time. He went through a month of not sleeping well due to stress, illness, life reasons. “I could barely function off nine hours of sleep for two years, and during the last five weeks’ time I was functioning on far less sleep!” Right now he feels so good, and is so happy, that he is scared to say it.
Adding more with zero repercussions, feeling better. He is inching his way back to the last good day in January 2024, when he went on two 45 min walks and ran for 60 seconds with his girlfriend. Yesterday went on two 45 min walks. Saturday night he went out to eat and was chasing his nephew around, which he did several times, picking him up, and not having negative repercussions.
The fiberglass pain is getting better. When that goes away he feels like a normal person.
“Finally all of the stuff I’ve been taking has been able to help in a way that I can feel.”
He is having future thoughts again of working out, and envisioning more work and more school. If his health is better, he will propose to his girlfriend.
He DC’d LDN because of the surgery, and didn’t go back on it because of money, but since we last talked he started it again.
Fiberglass pain is resolving.
“I’m type A, very disciplined.” He still eats whole food and veggies, avoids alcohol, and when he is healthy, once a month would like to have a drink of alcohol. He had two drinks in the last few weeks, including on his girlfriend’s birthday two weekends ago and enjoyed it. He realized in the beginning that alcohol made him feel better from a medicinal point of view, and so stayed away from it. He was in a social setting with friends and family and enjoying every minute of it. Once he feels the alcohol, he sets it down.
Next week is his Spring Break. He scheduled an ultrasound, and an eye appointment. He feels like he could run right now and handle it.
Discussion of Rapamycin for more rapid decrease of microclotting by promoting increased autophagy.
IMPRESSION: Recovered from most recent acute illness, with three in the last month. Functioning well despite decreased sleep. Credits the stent placement with the increased energy and the Lithium Orotate for increased resolution of the fiberglass pain.
PLAN: For paid subcribers only, sent via separate email.