Keep it moving – by Scott Marsland, FNP-C
[ad_1]
HISTORY
Are there boys who don’t like jokes about poop? I haven’t met them, and I wasn’t one of them. When I was a kid, we had Dr Seuss books, but Everybody Poops by Justine Avery had yet to be written. Honestly, I feel silly using the word poop, but I’m trying to keep this Substack at least PG rated.
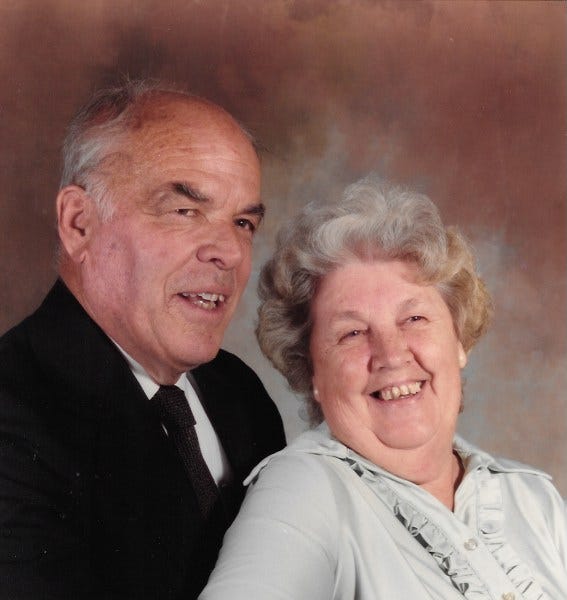
Poop was the word my stepfather Em instructed me to use. He landed in my life when I was eleven years old. Em was short for Embury. He was Embury T Jones, Jr, the only son of an engineer and inventor. He was a big man, 6’2”, 260 lbs of muscle, with a voice that carried the entire bass section of the men and boys choir of Christ Church Episcopal Church in Hartford, CT.
Em was a corporate headhunter, and a former computer scientist from when computers occupied entire buildings and used punch cards for programming. He was a Captain in the US Naval Reserve, who bounced a quarter on my bed to test whether I had tucked the corners tightly. He was, well, a Captain. If you didn’t like the way he ran his ship, you could walk the gangplank. He didn’t like swearing. We didn’t agree about what constituted swearing.
By fourth grade I was singing in the St James Episcopal Church boys choir in West Hartford, CT. Thus, Em and I would come to share a love of sacred choral music. The church choir was where I learned to swear, smoke cigarettes, drink alcohol, shoplift, and kiss girls. Not necessarily in that order, but all in the same year.
I shouldn’t blame all my vices on the boys choir. Swearing came naturally to me. I’ve always been small, so I made up for it with expletives. My elementary classmates from Cuba and Puerto Rico were more than happy to teach me swear words in Spanish. Enough to get cuffed by Mrs Rodriguez our Spanish teacher.
In prescience of the tumultuous relationship we would have, Em rescued my petulance tuckus years before he became my stepfather. St James choirs joined Christ Church Cathedral choirs for a special performance of …who knows what? I don’t remember the music. What I remember is that when the choirmaster from Em’s church saw me sticking my tongue out at the junior high hotty I had my heart on, he grabbed me by the scruff and tossed me in the stairwell. Ouch! Em came into the stairwell a few minutes later and made sure I was okay. I was just a tad humiliated, but otherwise figured all is fair in love and war.
So, swearing. There are so many words for human excrement. None are quite as definitive and satisfying as s**t. The French have merde. The Brits have shite. Under the house rules of Captain Jones, poop was permissible, crap was not, s**t definitely not. There would be consequences. A battle of wills ensued. Ultimately I walked the plank, and went to live with my Nana and Pop pop in another state. My grandparents thought they were going to enjoy their golden years in peace and instead ended up raising a teenager.
Pop pop was more my speed. A former US Marine who fought in Okinawa. He was a gentleman and had good manners, but he also knew his way around some serious vernacular. Heck, even my Nana would drop a s**t bomb now and again. In his later years Pop pop was bald on top with a horseshoe of hair. He ran a service station for forty-five years, and was happy to be under the hood of a car tinkering. Except that on more than one occasion he would bang his exposed scalp on the propped hood of said car, which would lead directly to a Pop pop classic: GOD…DAMN, goddamn, goddamn!
Pop pop’s objection to profanity was more about timing. Not a big deal to say s**t, but do we have to talk about it at dinner? Well, if you were me you did. Another battle of wills ensued, although better matched, as we were both Marsland men after all. An enlisted man couldn’t exercise too much probity.
RECENT HISTORY
My comfort level with expletives is a perfectly valid reason why I ended up working in the Emergency Department (ED). The floor nurses were really just too proper, and had a bit too much value judgement going on, perpetually. The ED was the realm of hoodlums, prisoners, homeless, drug users, and working folks in medical crisis. Do you think that patients with 10 out of 10 flank pain from kidney stones are focused on keeping their conversation Disney-appropriate? No. By the time I landed in a level 1 trauma center, it was generally a non-stop s**t show. F-bombs were de rigeur.
Fortunately for me and my patients, my familiarity and comfort level with s**t was more than vowel and consonant deep. Ask any nurse what her/his/their hot button body fluid is and you’ll get some interesting conversation going. I worked with a nurse, who shall remain named Chicken Nugget (you know who you are), and she has this super power of turning off her sense of smell when she starts a shift in the ED. She was impervious to s**t.
I’m not so lucky as Chicken Nugget, but my Kryptonite is sputum. One time when I was still sporting a crew cut, I was in an isolation room doing tracheostomy suctioning. The patient coughed a huge, green, sticky sputum clump that skidded across my scalp, slowly settling in for a landing. I could only finish the job I started as the goo slowly sank into my hair. So, sputum, no thanks. But vomit, urine, blood, sweat, tears, and s**t, no problem.
In fact, I’m so relaxed around s**t, that I developed a reputation for being a masterful disimpactor. I just made up that word, but that’s what I was good at. May you never have need of fecal disimpaction, but if the occasion did arise, you for sure want someone who brings plenty of lubrication, a sturdy constitution, a gentle and kind manner, patience, and long fingers. That’s me. When you’re the one experiencing a disimpaction, it’s very intense, but when it’s done well, you are very, very appreciative. No joke, I once had a grateful patient’s wife force a wad of hundred dollar bills down my scrub top after I got him unplugged. It’s a shame that I was a serf of New York State and couldn’t legally accept the tip. This is all to say that s**t happens, the ED is often a s**t storm, and a satisfying s**t is one of the elusive pleasures of a well-lived life. Now let’s talk about how to keep things moving.
PRESENT
As promised in my last Substack, I’m going to cover supplements and medications which are harmful in general, but specifically problematic in patients experiencing post-acute sequelae of Covid (PASC) and Covid vaccine injury. Last week I wrote about aluminum containing medications. This week I’d like to discuss polyethylene glycol or PEG.
Polyethylene glycol (PEG) is a petroleum-derivative compound that is made from ethylene glycol (ethane-1,2-diol), the main ingredient in antifreeze. PEG can be found in a number of other products, including skin creams and personal lubricants, and as a food additive for anti-foaming purposes. PEG may be familiar to you by its brand name MiraLAX. This is pure PEG crystals, sold over-the-counter, and marketed as a laxative. In 2019, the MiraLAX brand generated about 29.7 percent of laxative/stimulant liquid/powder/oil sales in the United States. Sales of laxatives in 2023 topped $1.5 billion annually, and apparently there is a shortage.
How does MiraLAX work? It is classified as an osmotic laxative. This means that it works by drawing water into the colon. The water softens the stool and may naturally stimulate the colon to contract. These actions help ease bowel movements.
If you have been using PEG for years, you are probably wondering what the fuss is about? This is a great example of the difference between the pre- and post- Covidian world. You know the song “The Old Gray Mare”? She ain’t what she used to be. These bodies we are living in are changed, with innumerable pathologies and complications to confound us.
The PEG story goes back to an important decision made by the Covid mRNA vaccine manufacturers. PEG-modification (pegylation) conjugates PEG with the lipid nanoparticles (LNP) in the shots. It coats the surface of the LNPs reducing opsonization, aggregation, and improving mRNA delivery to the target cells. Translated, it helps the LNP glide past our immune system surveillance and through the phospholipid membranes of our cells. This action enables longer circulation of nanoparticles. However, there is now evidence that PEG causes immunogenic responses when conjugated (PEGylated) with other materials such as proteins and nanocarriers. See studies here and here. It has been estimated that up to 25% of people who received a Covid shot have developed antibodies to PEG.
If we have learned anything from the censorship of HCQ, IVM and other repurposed drugs which could effectively treat Covid, we should bear in mind that the scientific literature on occurrence of PEG antibodies is compromised. When you read a study which minimizes this, i.e. concludes that PEGylation in the Covid shots is safe and effective, make sure to also read the conflicts of interest declared.
What happens when a person develops antibodies to PEG? If you are allergic to something, and you ingest a sizable quantity of it on a daily basis, it is going to make you sick. Signs of a new allergy to PEG include pruritus (itching), tingling, flushing, urticaria (raised, red welts on your skin), angioedema (facial swelling), hypotension, and bronchospasm.
Spike protein destabilizes mast cells provoking mast cell activation syndrome (MCAS) in many PASC and vax patients. When mast cells are unstable, they are frequently releasing histamine. Whereas white blood cells have a lifespan of about a week, mast cells last 2-4 years. We’ll be dealing with this dynamic for some time to come. In the context of MCAS, PEG antibodies mean that PEG-containing products have the potential to trigger anaphylaxis or hypersensitivity reactions in some people. In the most extreme of cases, a new PEG allergy has created enormous obstacles to treatment as there are many beauty care products, medications and even foods containing PEG. I have found this to be the case with more than six patients under my care. One patient would experience severe anxiety, tachycardia, flushing, and dizziness from the tiny amount of PEG in a dose of the anti-histamine Pepcid/Famotidine. My experience is that when patients wean off MiraLAX, there is a significant improvement in their global symptom burden.
Products containing Polyethylene Glycol
Medications using Polyethylene Glycol
Foods containing Polyethylene Glycol (See these WHO 2021 food additive details)
-
Emulsifiers, stabilizers and sweeteners
-
Chewing gum
-
Food supplements
-
Water-based sports, energy and electrolyte drinks
-
Surface treated fresh fruit
What now? Laxatives are habit forming. If you have come to rely upon MiraLAX/PEG to have regular bowel movements, it would be unwise to stop abruptly, even if you are slowly poisoning yourself. If you develop a small bowel obstruction and need emergency surgery, you haven’t gained any ground. A more strategic response is to wean yourself over several weeks and replace the MiraLAX/PEG with safer alternatives. My favorite supplement in this case is OxyPowder, a combination of ozone-oxygenated magnesium and citric acid. I also like to use Garden of Life Prebiotic fiber which you mix with water and drink. Metamucil is readily available in most grocery stores and pharmacies. Prunes are an old standby.
We also need a longer-term plan to get off the laxative train, but keep things moving. Regular bowel movements require three components: hydration, dietary fiber, and mobility. Just like a three-legged stool, if you take away one of those three components, it isn’t stable. Hydration can be the easiest part. More than twenty-five years ago, a college classmate of mine changed my life with some simple advice. It was Mohit Bali, an introverted computer major who was observant if not elegant in his delivery. He told me that every morning when I wake up, I should drink a big mason jar of water right away. He explained that this was a basic teaching of Ayurvedic medicine for more than 3,000 years, and would help me lead a long and healthy life.
What Mohit didn’t share, but which I later learned, is that every human being wakes up dehydrated. Our body spends the time we are asleep engaging in cellular repair, burning fuel, making waste, using up oxygen and water. What we do instead of hydrate upon waking? We drink coffee. Yes, it stimulates our bowels, but the caffeine is a diuretic, which makes us pee and dehydrates us further, so that we start the day deeper in the hole. If you must drink coffee, then have at it, but drink a 32 oz of water first thing and you’ll thank yourself for it. The water will also stimulate you to have a marvelous BM.
Mobility is the next challenge, especially if we have the fatigue and post-exertional malaise of PASC and vaccine injury. Simply put, moving your body stimulates gastrointestinal motility. Move your body less, and waste will take longer to pass through you, permitting more of the moisture to be reabsorbed by your intestinal walls, creating bigger and drier stool.
Obtaining dietary fiber is as easy or hard as you choose to make it. You can use the options I mentioned above, but food is best. There are two kinds of fiber: soluble and insoluble. Soluble fiber gives stools bulk. Foods that are good sources of soluble fiber include apples, bananas, barley, oats, and beans. Insoluble fiber helps speed up the transit of food in the digestive tract and helps prevent constipation. Good sources of insoluble fiber include whole grains, most vegetables, wheat bran, and legumes. Foods that have fiber contain both soluble and insoluble fibers.
Diametrically opposed to fibrous foods are processed foods. White rice, white flour, refined pasta, and sugar have the effect of gumming up the works. Minimizing these aspects of your diet, and maximizing whole foods will produce long-term health benefits and more regular BMs.
Water, movement and fiber. Drink water early and often. Happy trails to you.
P.S. I have no financial interest in the products which I recommend, such as OxyPowder, Garden of Life Prebiotic Powder, or Metamucil.
[ad_2]
Source link