[ad_1]
PAST
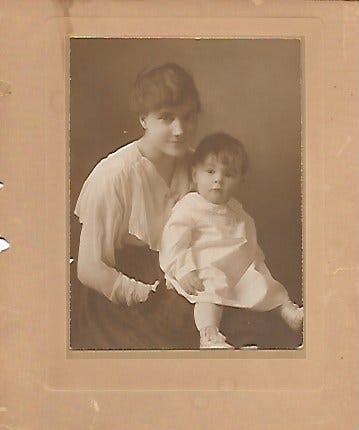
A refrain which I heard frequently as a child was that I was “just looking for attention.” I had some intuition that this wasn’t a bad thing, but it was framed as just that by some of the adults around me who had other interests besides paying attention to a little boy.
Fortunately for me, there were other adults who were happy to pay attention. This included dozens of grey and white-haired customers on my paper route, my paternal and maternal grandparents, and my godparents. There was enough collective attention among them that I emerged from childhood without getting picked off by some predator who could smell the attention-starved boys and girls like a fox smells the rabbit.
When I was fourteen years old, my friend Larami’s parents sponsored me to go to a weekend workshop for young people. It was my first introduction to Re-Evaluation Counseling or RC, was held in a big old house in West Philadelphia, and led by an RC leader named Blair Hyatt. Larami was there too, as was another high school classmate named Tracy, and about a dozen other teenagers. That weekend changed my life, and how I thought about people—and attention.
The way these workshops go, each person gets a turn, if not multiple turns, in front of the group with the leader paying attention to them. Even the leader takes a turn. This last piece is important, because, unlike most conventional therapies in which the therapist is positioned as the knowing one, within RC, the leader has the opportunity to share their struggles with their community. It’s a different model of leadership, which has pluses and minuses, and doesn’t necessarily translate to the non-RC world.
One thing which I learned that weekend was that no matter how confident and together someone looked on the outside (e.g. Tracy), everyone had an interior emotional life, insecurities and old hurts that they were handling. This became clear to me as we took turns listening to each other in small groups as well as the entire group. The stunning moment was when Tracy was in front of the group with Blair paying attention to her in a light and playful way, and she burst into tears. I remember thinking, “What the hell just happened?” I didn’t expect this, and somehow the attention of Blair and the group made the difference. Tracy showed herself in a way that I hadn’t seen in the two years I had known her, and it made me care more deeply about her.
Another very important thing which I learned that weekend was that we all want and need attention, but that things go much, much better if we take turns. This immediately made sense to me. How many times have we been in a conversation where everyone is chomping at the bit to speak, and not necessarily listening to what the other people are saying? RC explicitly circumscribed this approach, by using timers, with each person taking a turn as client and counselor. You could begin to let go of formulating what you wanted to say while someone was still speaking, because you knew that your turn would come.
Perhaps the most important thing I learned that weekend though, was that I was a good listener, and that my listening could help another person to heal. People at that workship, and in RC over the years, showed me how to use attention to examaine what has been hard in life, with the aim of moving through it and moving on from it. I felt like I had discovered a superpower. We all have a need to be loved, but I would assert that our need to demonstrate our love for others, is far greater. RC presented me with a way to do this regularly, and skillfully.
RECENT PAST
One of the best decisions I ever made was to get a vasectomy in my mid-twenties. (I didn’t yet know that vasectomies don’t prevent you from adopting large numbers of cats, but that is a story for another day). For a year and a half I had been living together with the woman who would become my wife. I was still swearing that I would never get married, but was even more certain that I didn’t want to have children. She wasn’t as fervent on the issue of kids, but we both had come from broken homes, and had serious doubts about our capacity to be good parents. And so we came to an agreement that I would get fixed. So out-of-the-norm was this desire, that it took another year for my primary doctor to agree to sign off of the surgery, as he wanted me to take a year to “think about it.”
At this point in life, I don’t doubt that my wife and I could be good parents, if only because we have spent so much time raising each other into adulthood, and becoming relatively balanced human beings. But I’m still glad that we didn’t become parents. What we have had as a child-free couple is fewer financial constraints, more time, and freedom.
Parenthood doesn’t have to be the death of romance in coupledom, but it sure seems to be a common side effect. You can read romance to mean not just a sex life, but also closeness, connection and a fighting chance at finding intimacy, whatever that elusive relational state may be for you.
As a child-free couple, we have been able to step up during some very important times in the lives of our extended family. When my sister-in-law was in the hospital for a major surgery, I was able to take time off from work to help watch my three nieces while my brother worked long hours at a demanding job in finance. When my father was dying of metastatic kidney cancer, we were able to regularly drive five and a half hours to his home, and provide respite to my stepmother during the last months of his life. We did this at a time that we were both working retail jobs, didn’t have a car (we would rent one) and with finances that were very tight. When my paternal grandmother was dying from colon cancer, and had burned her bridges with my aunts and uncles, we were able to take her into our home and care for her during her last month of life. Each of these experiences was deeply meaningful and had its own intrinsic rewards for us, but I know also made a big difference for those receiving our time and attention.
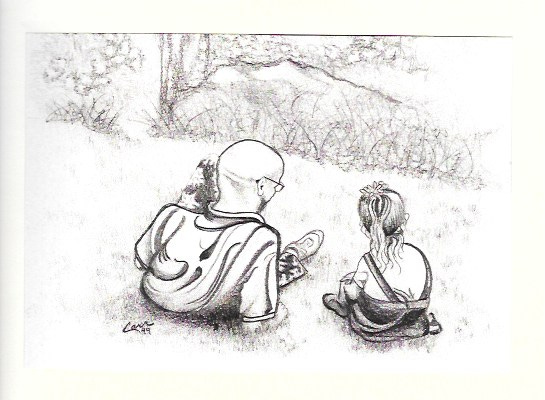
My wife learned RC when we first moved in with each other in 1994, and quickly became a skillful counselor, better than me in fact, even though I had been at it a decade longer. We tried to use our super powers of attention to elevate the emotional lives of our nieces and nephew. We’ll never know what impact those efforts had, but we quickly understood the limitations of our influence, as parents often seen their children as their private property, and can quickly perceive competition and threat from other adults who have relaxed attention for them.
One summer we had two of our nieces come to visit us in Ithaca, NY and had a memorable week hiking, camping, and exploring together. My brother and sister-in-law expected the girls to be homesick, and were miffed when they didn’t get a call which affirmed this. The week was not without its challenges, as our nieces tested us and used our attention to show some of the struggles they had, but couldn’t get air time on at home. I think that all of us had a sense of closer connection to each other by the end of the week, and my wife and me were looking forward to another visit the next summer. When we later asked about having the girls come visit again the next summer, we were told that they would be going to camp. I suspect we did not get that opportunity again because my brother and sister-in-law perceived a threat to their parental exclusivity and validity.
Given what I have learned about attention, giving and receiving, and the healing power of it, I’ve long thought that many people shouldn’t become parents, or at least not as soon as they do. All humans need attention, but children especially. How rational is it that people become parents when they haven’t developed their capacity to pay attention to others? As far as I can tell, good parenting is more likely to flow from adults who have some capacity to meet their own human needs, including self-validation, without needing to extract it from the dependent little creatures they brought into this world. I have come to believe that developing our capacity to pay and share our attention can only improve our interactions with each other, and the children in our lives.
PRESENT
As a Family Nurse Practitioner, I was trained in delivering care to human beings from birth to death. If I had to, I think that I could do a decent job of delivering a child, but I’d rather not. I’ve cared for plenty of children during years of work in an Emergency Department which treated children and adults, but pediatrics isn’t my favorite. Yet, due to the uniqueness of thess post-Covidian time, there have been teenagers and pregnant women who have needed my care.
The most frequent appearance of pregnancy in my practice with the Leading Edge Clinic has been after a miscarriage or stillbirth. Women and couples who are seeking to understand what about COVID or the COVID shots is interfering with successful pregnancies seek out our counsel. I think that we have some insights into the pathology of the spike protein which have been helpful in those cases.
In one instance, a young woman who had started treatment for injury from the COVID shots, was due for a second visit, and became pregnant in the interim. During our second visit, I met with this patient and her husband, and the focus was on how we should modify her plan of care now that she was pregnant, and specifically, whether or not she should keep taking Ivermectin.
Medicine is perpetually an enterprise of risk vs benefit. What we witnessed in the last four years was the utter abandonment of informed consent, which cannot occur in any meaningful way without discussion of risks vs benefits of different treatment options. In discussing the use of IVM with this couple, I explained that there was some evidence of teratogenic effects (birth defects) of IVM in the first trimester, but at doses which were also harmful for the mother. We have been treating patients with IVM since February 2022, and I haven’t seen worse than blurred vision or GI upset in a minority of patients, despite doses as high as 0.6mg/kg. (There were two patients who were self-described as very sensitive to everything, who had what I would describe as Herx reactions upon initiation of IVM dosing, even at 1mg per day, but they were extreme outliers).
This particular patient had stopped IVM when she learned that she was pregant. She was taking only 2mg per day, which is far lower than I use in most patients, but she was also a self-described sensitive patient. Within three days of stopping IVM, the symptom of dizziness which had been plaguing her prior to taking IVM, returned.
To counterbalance our discussion, I asked the rhetorical question: “Have you been told that it is safe to take Tylenol (Acetaminophen) in pregnancy?” Yes, they had been told that it was safe. I then relayed my understanding of acetaminophen’s safety— or lack therof. For purposes of this Substack I’ll stick with the less impressive, but also less debatable numbers. According to the CDC, 1567 people have died from accidental Tylenol overdose between 2001-2010. During that same time period, annual acetaminophen-related deaths amounted to about twice the number attributed to all other over-the-counter pain relievers combined, according to the poison control data. A 2018 study published in a Scandinavian journal reported acetaminophen poisoning was associated with increased long-term all-cause mortality. The increased all-cause mortality was more prominent in the younger population, and in the first 12 months after poisoning. In July of 2009, an FDA panel of thirty-seven experts came very close to issuing a call for a ban on all over-the-counter sales of acetaminophen to reduce associated deadly overdoses and to eliminate the leading cause of liver failure in the U.S. They instead pulled back and called for only limiting the amount of Tylenol used in combination with narcotics such as Percocet. A 2023 study found that this decision saved many lives. This 2013 report from ProPublica does a good job of chronicling the sordid and deadly history of acetaminophen, and Big Pharma’s dodginess in response to decades of efforts to curtail its over-the-counter availability and use. However, it is still widely considered safe to use in pregnancy.
Now, let us again consider IVM. In 2021, a French company which had developed a long-acting, injectable form of IVM, commissioned a sweeping study of the medical literature on IVM by the well-respected French Toxicologist, Dr Jacques Descotes. He examined 82 chapters in multi-authored books, 249 original scientific papers, 74 review papers in peer-reviewed journals, 486 presentations and posters at scientific meetings on the preclinical and medical safety assessment, immunotoxicology and immunological safety, regulatory safety and risk evaluation of medicinal products and chemicals. In more than three decades of use, in hundreds of millions of people, there wasn’t even a solid case to be made that IVM was associated with a single death. He concluded that “…the safety profile of ivermectin has so far been excellent in the majority of treated human patients so that ivermectin human toxicity cannot be claimed to be a serious cause for concern.”
I know which of these two products I would feel comfortable recommending for use in pregnancy.
A 2020 systematic review funded by Unitaid (read Bill Gates) found: “There is insufficient evidence to conclude on the safety profile of ivermectin during pregnancy. Treatment campaigns should focus additional efforts on preventing inadvertent treatment of pregnant women.” I find it noteworthy that the recommendation is to prevent inadvertent treatment rather than more closely study its safety in pregnant women, and the authors take pains to point out the low quality of the studies used.
No evidence was found for increased risk of neonatal deaths, preterm births or low birthweight. Some evidence was found for spontaneous abortions, stillbirths, and congenital anomalies, but the number of cases was too low to be conclusive – fewer than 100 women were exposed during the first trimester, when the foetus is expected to be more vulnerable to the drug’s effect.
Alternately, in its discussion of the Unitaid (Gates) review, the Barcelona Institute for Public Health spends a moment longer on the pertinent point that if IVM could be shown to be safe in pregnant women, that would be very important for public health. That is because IVM is not only used to treat the parasitic infections of onchocerciasis, lymphatic filariasis, Strongyloides, and scabies, but also has potential role as an endectocide to reduce malaria transmission by killing malaria vectors. The consensus of scientists and public health workers is that malaria kills up to 2.7 million persons each year. Nine out of ten of these cases and deaths occur in Africa and the vast majority of them are in children under the age of five years. If IVM got the green light for use in pregnancy, it could save many more lives.
The introduction to the Unitaid (Gates) review is worth quoting in detail; highlights are mine.
Before moving to the narrative description required by the 2015 labelling rule,9 the US Food and Drug Administration (FDA) had previously classified ivermectin as pregnancy category C—ie, “Animal reproduction studies have shown an adverse effect on the foetus and there are no adequate and well-controlled studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks”.1 This classification is based on studies done in mice, rats, and rabbits during the original New Drug Application in the 1990s by Merck (appendix p 2).10 These studies showed adverse pregnancy outcomes at cumulative doses that are high enough to produce signs of maternal toxicity in animals, ranging between 20 and 600 times the human Mectizan single-dose target of 0·15–0·20 mg/kg. However, later evidence showed that the mouse strain (CF-1) used in the initial acute and developmental ivermectin toxicity studies was inappropriate, as it was later shown that CF-1 mice have deficient P-glycoprotein expression, which is an efflux pump key to preventing ivermectin toxicity.11
My interpretation of the above is as follows. First, if we were to dose a pregnant human female at 20 to 600 times the typical single-dose use of 0.15-0.20mg/kg, for a 120lb (54.5kg) woman, instead of 12mg, we would use doses of 1090 – 6540mg. That ain’t happening. Second, the mouse studies which demonstrated teratogenicity to the fetus used a type of lab mice which have a genetic mutation that leaves them unable to avoid IVM toxicity. Hmmm.
I’ll report that in our clinical experience, whether a person has received the COVID shots or not, all of our patients have amyloid fibrin microclotting. If a person received two or more shots, they will typically have microclotting stage/grade 3-4 on a scale of 0-4. We know that microclots concentrate in the capillaries, where red blood cells (RBCs) are meant to deliver oxygen and remove carbon dioxide, but can’t due to congestion and blockage. We also know that the dense networks of blood vessels within the placenta are responsible for exchanging respiratory gases, nutrients, and wastes between the mother and fetus throughout pregnancy, which is essential for proper fetal growth. And we know that IVM is very effective at blocking the clot- provoking impact of spike on the platelets, RBCs, and endothelial cells which line the blood vessels.
In a post-Covidian world, the risk of using IVM in pregnancy is inhibited by the inconclusive and weak body of evidence (per Unitaid (Gates)), and studies using mice which couldn’t avoid IVM toxicity at crazy high doses. On the other hand, we have a punctilious review by an esteemed toxicologist, basically saying that IVM hasn’t killed anyone over thirty years and hundreds of millions of doses. And our clinical experience reveals microclotting in everybody, which poses an imminent threat to the viability of a fetus. IVM is one of the most effective therapies to block that effect of spike to promote microclotting.
If it was my wife who was pregnant, after a detailed review of the above risks and benefits, I would opine that I think the risks of IVM at current dosing at 0.2mg/kg-0.6mg/kg for post-acute sequelae of COVID and COVID vaccine injury are not only safe in pregnancy, but likely to prevent fetal demise from microclotting. If my wife was especially sensitive and cautious, I would use as little as 1mg of IVM daily, but I would use it.
P.S. This Substack is not individual medical advice for you.
P.S.S. Happy Memorial Day!
P.S.S.S. Thank you to each of the paid subscribers who help support the long-term effort of writing.
[ad_2]
Source link